Cardiovascular disease (CVD) is the leading cause of death for women globally. In Europe, CVD accounts for 45% of deaths in women and 39% of deaths in men.1 In the US, between 1994 and 2020 mortality due to CVD decreased in both sexes, but less for young women (≤55 years) compared to young men.2 Advances in therapeutic options have contributed to these improvements. Each year in the US, it is estimated that >600,000 percutaneous coronary intervention (PCI) procedures are performed, of which approximately one-third are performed in women.3 However, despite improved clinical outcomes following PCI with a contemporary drug-eluting stent (DES) in patients with ischaemic heart disease (IHD), worse outcomes have been described in women.4–6 Further, whether PCI-related outcomes vary between women and men according to age, race, clinical presentation or type of stent remains poorly understood. Controversial data have been reported after adjusting mortality by age and comorbidities in patients subjected to PCI in several settings.3,4,7 Other factors also contribute to the disparities between sexes.6,7 For example, coronary arteries in women tend to have smaller body size-adjusted diameters and more tortuosity, and are more prone to dissection and perforation, with a consequently higher risk of coronary stent late lumen loss.8 Moreover, women are less likely to receive guideline-recommended PCI for IHD than men. In addition, women have a higher risk of vascular access site complications and periprocedural bleeding.7 However, the effects of sex on clinical outcomes under concurrent PCI have not been fully clarified as yet.4–8
The main aim of this review is to summarise the current evidence on sex-related differences in patients with IHD, focusing on differential outcomes following PCI in different scenarios. This research adds to the recent literature specifically on differences in PCI outcomes in different scenarios, namely acute coronary syndrome (ACS), stable angina and technically complex coronary lesions, with a critical perspective on the current literature, and highlights the gaps for future research on this topic.
Sex Differences in the Epidemiology of Acute Coronary Syndromes
ST-elevation MI (STEMI) and non-STEMI (NSTEMI) account for approximately 30% and 70% of ACS in women, respectively.10 After 65 years of age, significant decreases in all acute MI (AMI) types have been observed for women in high-income countries.7,8 However, the annual incidence of hospitalisations with AMI has increased for younger women (≤55 years).11,12 For example, in a large French nationwide study performed from 2004 to 2014, the rates of age-standardised admissions for ACS in patients younger than 65 years increased by 6.3%.11 This rise in ACS was driven by significant increases in STEMI (+21.7%) and NSTEMI (+53.7%).11 Smoking and obesity were significantly associated with the observed increase in STEMI in younger women.11
Percutaneous Coronary Intervention Outcomes in Women with Acute Coronary Syndromes
ST-Elevation MI
Sex differences in the provision of invasive management of ACS have been described in observational clinical studies.11–15 It has been shown that women are less likely to undergo reperfusion therapy after ACS (adjusted OR for PCI 0.68; 95% CI [0.66–0.70]).15 Although some of the discrepancies between the sexes in the provision of invasive therapy may relate to differences in age and comorbidity, differences persist even after adjustment for age and comorbidities. This attitude is persistent and yet unexplained. In a Spanish study conducted from 2003 to 2015 including 277,281 patients (29% female), women were less likely than men to be treated with primary PCI.13 Although the use of PCI increased in both sexes from 2005 to 2015, specifically from 56.6% to 75.6% in men (IRR 1.02; 95% CI [1.02–1.03]; p<0.001)] and from 36.4% to 57.0% in women (IRR 1.04; 95% CI [1.04–1.05]; p<0.001), discrepancies remained between the sexes.13
Women with STEMI after coronary revascularisation have higher unadjusted hospital mortality than men, more often experience bleeding complications and have up to 30% more readmissions within 30 days.16–20 A meta-analysis of more than 50,000 patients (18,555 women) with STEMI undergoing primary PCI reported a higher risk for in-hospital mortality (RR 1.93; 95% CI [1.75–2.14]) and 1-year all-cause mortality (RR 1.58; 95% CI [1.36–1.84]) in women compared with men.21 The incidence of cardiogenic shock complicating STEMI is also higher in women than in men, but the use of PCI in this setting is less common in women than in men, despite randomised control trial evidence of equal benefits.16,17,22–24
Non-ST-elevation MI
The treatment of patients with unstable angina (UA)/NSTEMI is more complex and challenging than the treatment of patients with STEMI. In STEMI, differences in outcomes are largely age and sex-dependent, with worse outcomes seen in young and middle-aged women.25,26 In UA/NSTEMI, clinical presentation is the key factor influencing outcomes. Ischemic risk should be categorised at admission and may influence decisions regarding management.27,28 However, in patients with NSTEMI, the European Society of Cardiology and American Heart Association/American College of Cardiology guidelines do not suggest stratification of risk based on sex.27,28 These guidelines suggest that patients at very high risk are likely to benefit from immediate invasive therapy, whereas the decision in low-risk and intermediate-risk patients is more nuanced.27,28
RCTs examining the management of NSTEMI in women have shown divergent results. For example, in the RITA 3 trial (n=1,810 patients; 682 women), researchers found that the incidence of death or MI after 1 year was higher in men allocated to conservative therapy than in the intervention group (10.1% versus 7.0%; adjusted OR 0.63; 95% CI [0.41–0.98]).29 Nonetheless, the death and MI rates at 1 year in women were similar in the conservative therapy and intervention groups (5.1% versus 8.6%, respectively; adjusted OR 1.79; 95% [CI 0.95–3.35]; p for interaction=0.007).29 For men and women in the low-risk group, rates of death or MI were similar in both the intervention and conservative therapy groups (6.1% versus 5.1%, respectively, for men; 2.3% versus 3.8%, respectively, for women). However, among patients at moderate and high risk, women in the intervention arm experienced a higher event rate of death or MI than those in the conservative therapy arm (13.4% versus 3.4%, respectively, for moderate risk; 11.7% versus 8.2%, respectively, for high risk).29
A meta-analysis of RCTs comparing an early invasive strategy and a conservative treatment strategy in patients with NSTEMI and UA found that men and high-risk women did not benefit from an early invasive strategy.30
Conflicting results have been reported regarding differences between the sexes in the use of an early invasive strategy in the setting of NSTEMI.30,31 An analysis of the National Inpatient Sample databases for non-ST-segment-elevation acute coronary syndrome (NSTEACS) found that women experience higher in-hospital mortality than men in unadjusted models, but have a 10% lower risk of mortality after multivariable adjustment.31
Conversely, recent large studies have shown increased mortality in older men, but not in women of any age, presenting with NSTEMI.20,25
Key Considerations for Using Percutaneous Coronary Intervention in Women and Delays to Angiography
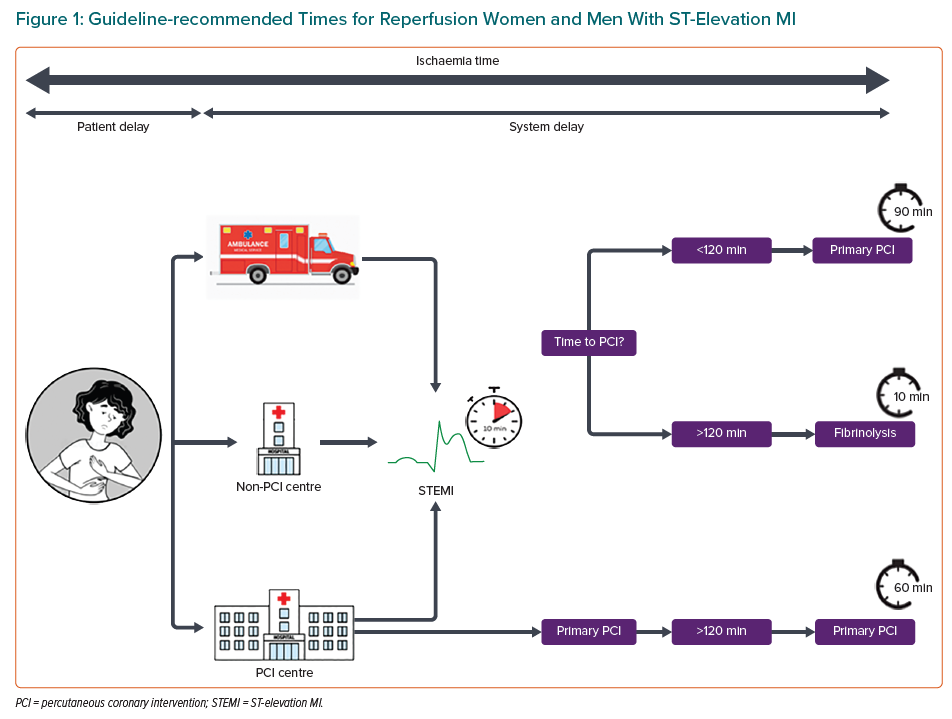
Compared with men, women with STEMI tend to present later after symptom onset and tend to experience both longer delays even after arriving at the emergency department, including longer triage and door-to-balloon times, and lower rates of guideline-directed medical therapy, which may contribute to poorer outcomes (Figure 1).32-34
Among patients who have sought medical attention for symptoms before ACS onset, women are more likely to have been offered reassurance by clinicians that their symptoms were non-cardiac in origin (53.4% versus 36.4%; p<0.001).35 Although chest pain appears to be present in approximately 90% of patients with MI regardless of sex, women tend to present with a more diverse symptom profile.36 Other reasons for the greater delay in seeking medical attention among women than men include lack of awareness, previous barriers to accessing care, fear, embarrassment and previous misdiagnosis of their chest pain by a health professional.36 There are also important system factors at play. Although recent data have shown that women are less often transferred by network systems to primary PCI centres than men, the introduction of network systems was related to an increased provision of primary PCI and was associated with reduced in-hospital mortality in women.13,35,36
Assessment and Diagnosis of Acute Coronary Syndrome
High-sensitivity troponin concentration thresholds for NSTEMI diagnosis may be less sensitive in women than in men, and higher levels of high-sensitivity cardiac troponin (hs-cTn) have been recommended to diagnose MI in women.37 In a recent study including 48,282 patients (47% women), the use of the hs-cTnI assay with sex-specific thresholds increased the diagnosis of myocardial injury in women by 42% and in men by 6%.37 Yet, following implementation of the revised hs-cTn thresholds, women with myocardial injury remained less likely than men to undergo coronary revascularisation (15% versus 34%).37 However, it is relevant to remark that myocardial injury does not necessarily mean ischemic injury. Therefore, the use of sex-specific thresholds identified five times more additional women than men with myocardial injury.37 Despite this increase, women received approximately one-half the number of treatments for coronary artery disease as men, and outcomes were not improved.38
Antithrombotic Treatment
Regardless of a patient’s sex, the use of contemporary potent antiplatelet therapies has reduced the risk of both major adverse cardiovascular events (MACE) and all-cause mortality in patients with stable and unstable coronary disease, but with an increased risk of bleeding.27,28 Recent registry analyses have shown that patients treated with prasugrel or ticagrelor are more likely to be men.39,40 A meta-analysis of phase III or IV RCTs of potent P2Y12 inhibitors (including prasugrel, ticagrelor and intravenous cangrelor) included seven trials (24,494 women, 63,346 men).41 Potent P2Y12 inhibitors significantly reduced the risk of MACE by 14% in women (HR 0.86; 95% CI [0.78–0.94]) and by 15% in men (HR 0.85; 95% [CI 0.80–0.90]; p for interaction=0.93).41 Treatment with potent antiplatelet agents reduced the risk of MI by 13% in women (HR 0.87; 95% CI 0.78–0.96) and by 16% in men (HR 0.84; 95% CI [0.77–0.91]; p for interaction=0.65), and the risk of stent thrombosis by 51% in women (HR 0.49; 95% [CI 0.37–0.65]) and by 41% in men (HR 0.59; 95% CI [0.42–0.84]; p for interaction=0.85).41
Other Considerations Regarding Worse Prognosis in Women with Acute Coronary Syndrome
Worse in-hospital mortality rates are partially due to the fact that women with MI tend to be older and have more comorbidities than men, including hypertension, diabetes, renal failure, previous stroke, previous angina and heart failure, at the time of admission.13,22 Specifically, in women with diabetes and MI, mortality rates are higher than in men for all age groups except for those older than 80 years of age.42 However, even when adjusting for comorbidities and treatment differences, women tend to have a worse prognosis than men, and in some cases, could be linked to pathophysiological differences.18
Women presenting with ACS are at higher risk of major bleeding, which is related, in part, to inappropriate overdosing of antithrombotic therapy. A registry study including 23,473 patients with ACS found higher rates of bleeding and blood transfusion in women than in men (12.8% versus 7.3%) in the coronary revascularisation group.43 The increased use of vascular closure devices and radial access may further reduce these risks.44 These facts emphasise the importance of careful consideration of weight and renal function when selecting antithrombotic dosing to reduce bleeding, particularly in women, because despite adjusting antithrombotic treatment, women could be more vulnerable to bleeding complications. Further research into optimising bleeding avoidance strategies with a particular focus on women is warranted.
Percutaneous Coronary Intervention Outcomes in Women with Stable Coronary Disease
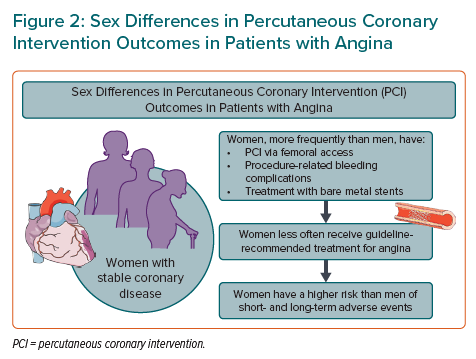
Although guidelines for stable angina do not differ by sex, women with angina and significant obstructive coronary disease less frequently receive guideline-recommended invasive treatment with PCI.45 Furthermore, drug-eluting stents are less frequently used in women than men, especially in women aged ≥75 years, despite evidence of improved outcomes compared with bare metal stents (Figure 2).4,46,47
Women are more likely to experience a higher symptom burden of angina than men and a subanalysis from the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial showed that patients with more frequent angina had greater improvements in quality of life when randomised to the invasive strategy compared with medical treatment alone.48–50
When they are treated with PCI, women tend to be older than men, with more cardiovascular risk factors.4,51,52 In two major PCI registry studies, Heer et al. (n=185,312; 28% female; 27% angina diagnosis) and Murphy et al. (n=54,440; 24% female; 23% angina diagnosis) found that women were more likely to have femoral artery access for the intervention, more frequently experienced major bleeding complications and less frequently had multivessel disease compared with men.51,52
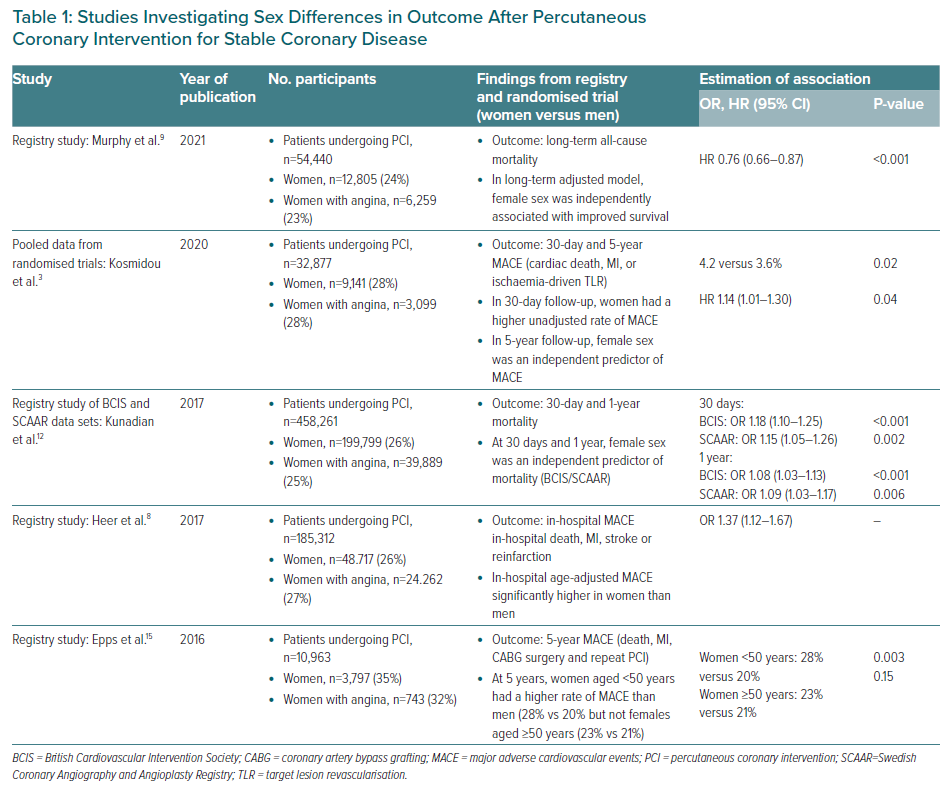
Several studies have shown that women who undergo PCI for angina have worse short-term MACE and all-cause mortality than men, although this may relate, in part, to differences in baseline characteristics (Table 1).52–54 Yet, in an adjusted analysis of British and Swedish registry data (n=458,261; 26% women; 33% angina diagnosis), female sex was independently associated with all-cause mortality at 30 days and at 1 year following PCI.53 Importantly, procedure-related complications were significantly higher in women.48 The prospective observational multicentre PLATINUM Diversity Study (n=4,182; 44.5% women; 26% angina diagnosis) reported a higher adjusted risk of 1-year all-cause mortality or MI among women than men.55
Disadvantaged outcomes have been confirmed in some RCTs for ACS presentations, but interestingly not in stable IHD: an individual patient data pooled analysis of 21 trials (n=32,877; 27.8% female; 33.8% angina diagnosis) showed that at 5 years after PCI, women had a higher risk of MACE and ischaemia-driven target lesion revascularisation than men. 4
Over the longer term, adverse outcomes for women compared with men could relate, in part, to differences in age, but data on this are conflicting. In a PCI registry study (n=10,963; 34.6% female; 39.4% with angina diagnosis), women aged <50 years had a higher risk of MACE at 5 years than men, whereas there were no sex-based differences in MACE for older patients.56 Furthermore, in a study of a predominantly older population with angina, women (mean age 71 years) had better long-term survival than men after adjusting for differences in baseline characteristics and interventions.52
Sex Differences in the Complexity of Percutaneous Coronary Intervention
Anatomical and lesion complexity affect outcomes after PCI. Although there is no standardised definition of complex PCI, certain characteristics of the coronary anatomy and the target lesion are known to represent a challenge for the interventional cardiologist and have an impact on peri- and post-procedural outcomes. These include multivessel disease with multiple lesions treated and/or multiple stents implanted, bifurcation lesion requiring two stents, chronic total occlusion or total stent length >60 mm, severe calcification, extensive thrombus burden, extreme tortuosity or a degenerated saphenous venous bypass graft as the target lesion.57 The evolution of PCI, including the introduction of DES, has occurred over past decades and has resulted in an increased number of patients with these lesion characteristics undergoing PCI. Depending on the definition, approximately 30% of PCIs are considered complex and, of these, approximately 25% are performed in women.57,58
Sex-specific Prevalence of Lesion Complexity
In general, women have been reported to less commonly have complex coronary artery disease than men. Data from a high-volume PCI centre registry showed that 54.9% of women fulfilled only one criterion for complexity, compared with 51.0% of men (p=0.02), whereas 27.8% of men fulfilled three or more criteria, compared with 24.1% of women (p=0.01).58 A pooled patient-level analysis of 21 RCTs of PCI found that 3.7% of women and 4.8% of men had three or more lesions treated and that the total stent length was significantly less in women than in men.4 Results from the WIN-DES collaborative patient-level pooled analysis (an all-female database with 11,557 participants undergoing PCI with stent implantation) showed that 18.7% had at least one bifurcation lesion.47 In the SYNTAX trial, an RCT comparing PCI and coronary artery bypass grafting (CABG) surgery in patients with de novo three-vessel disease and/or left main coronary artery disease, and therefore a population with complex coronary artery disease, only 22.3% were women.59 Compared with men, women had a lower SYNTAX score (mean 29.2 ± 11.1 versus 27.0 ± 12.2; p=0.001), lower rates of any total occlusion (24.7% versus 18.1%; p=0.006), lower rates of any bifurcation (74.4% versus 66.8%) and were treated with shorter total stent length in the PCI arm.59 Although these studies all indicate less complex coronary artery disease in women, it is important to keep in mind that women are less likely to undergo coronary angiography. Older age, renal dysfunction and other comorbidities contribute to the lower likelihood of women receiving coronary angiography than men. Therefore, the data that we have are limited to the women who are undergoing invasive evaluation of the coronary anatomy and are likely to underestimate the true prevalence of complex coronary artery disease in female patients. In addition, women tend to have smaller coronary arteries and more diffuse disease, which also represent challenges for the interventional cardiologist, even though these criteria are not usually included in the definitions of complex PCI.60,61 Another important consideration is the fact that among ACS patients, those with NSTEMI are more likely to have multivessel disease and complex coronary artery disease than those with STEMI, and women are more likely than men to present with NSTEMI. 62–65
Sex-specific Outcomes After Complex Percutaneous Coronary Intervention
Data on sex-specific outcomes following complex PCI are limited. With regard to periprocedural complications, an observational study on patients undergoing rotational atherectomy found that women more often experience coronary dissection, cardiac tamponade and significant bleeding, but with no impact on long-term survival.66 Similarly, a sex-specific subanalysis of the ORBIT II study in patients undergoing orbital atherectomy found that women more often than men experience severe dissections.67 Rates of other procedural complications were low, with no significant sex differences in perforation, persistent slow flow, persistent no reflow or abrupt vessel closure.67 In an analysis from the National Cardiovascular Data Registry on procedural outcomes of chronic total occlusion PCI, female sex was not a predictor of procedural complications.68
There are limited data on sex-specific outcomes following complex PCI. The analysis from the high-volume PCI centre registry mentioned above found that periprocedural complications occurred frequently with complex PCI, especially in women, who had higher rates of periprocedural MI (8.0% in women versus 6.0% in men; p=0.02) and coronary artery dissection (7.4% in women versus 4.1% in men; p<0.001).58 Women also had higher rates of periprocedural bleeding and blood transfusion regardless of PCI complexity. At 30 days, the adjusted risk of MACE (all-cause mortality, MI and target vessel revascularisation) was significantly higher in women than in men among those that underwent complex PCI (2.9% versus 1.3%, respectively; p<0.001; adjusted [a] HR 1.62; 95% CI [1.04–2.52]), but not in the non-complex PCI group (1.4% versus 1.1%, respectively; p=0.31; aHR 0.98; 95% CI [0.72–1.33]), with a significant interaction between sex and PCI complexity (p for interaction=0.04).58 The adjusted 1-year risk of MACE was similar between the sexes regardless of PCI complexity. An analysis from the all-female WIN-DES database revealed that complex versus non-complex PCI was associated with a significantly higher risk of MACE (defined as a composite of all-cause mortality, MI or target lesion revascularisation) and mortality at 3 years.69 Regarding long-term outcomes, the SYNTAX investigators found that female sex was not a predictor of mortality at 10 years in patients with complex coronary artery disease.59 The significant interaction between sex and treatment strategy at 4 years, suggesting higher mortality in women compared with men in the PCI but not CABG group, was no longer evident.70
High-risk Complex Percutaneous Coronary Intervention
Although women undergoing PCI generally have less complex coronary lesions than men, they also tend to have a higher risk profile due to older age and a higher prevalence of comorbidities, which means that women with complex coronary artery disease are more likely to be deemed ineligible for CABG.71 PCI with mechanical circulatory support may be an alternative for these patients. In a recent analysis from the CVAD registry, including 1,053 high-risk patients who underwent complex PCI with mechanical circulatory support using Impella 2.5 or Impella CP, only approximately 25% were women.72 Women had favourable outcomes after high-risk complex PCI with the use of mechanical circulatory support, more similar to men.
Percutaneous Coronary Intervention in the Left Main Coronary Artery
Several large RCTs have focused on the management and outcomes of PCI to treat unprotected left main coronary artery (ULMCA) disease, but women were underrepresented. For example, in the SYNTAX trial, women with ULMCA disease accounted for only 10.3% of participants, and those undergoing PCI had a higher adjusted 4-year mortality rate compared with men.73 In that study, CABG outcomes did not differ between sexes, and there was no interaction between sex and percutaneous treatment outcomes at the 10-year follow-up.59,70 In the EXCEL trial, 23.9% of participants were female.74 Although sex was not an independent predictor of adverse events after PCI, a trend towards worse outcomes was identified in women, related to more frequent pre-existing comorbidities and periprocedural complications.74 In the PRECOMBAT trial, 23.5% of participants were female, and no significant interactions between sex, treatment strategies and outcomes were reported.75
The few RCT data available are conflicting, whereas more specific information has resulted from several meta-analyses, trial substudies and registries. Interestingly, the vast majority convey concordant information regarding female patients’ baseline conditions, periprocedural complications and overall outcomes, and insist on the need for a deeper insight into sex differences in the management of ULMCA disease in women.
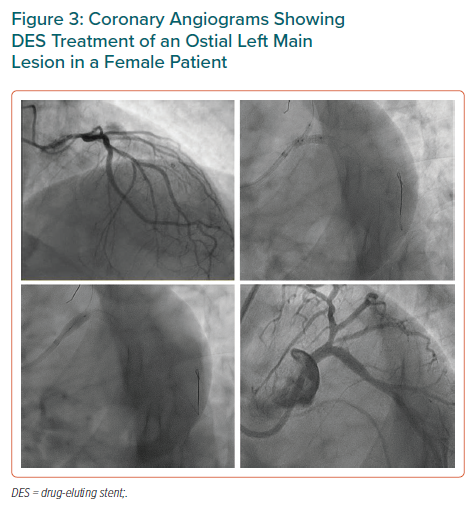
Women treated for ULMCA disease are generally older and more frequently affected by diabetes, hypertension and chronic kidney disease; they present more frequently with ACS and require more periprocedural haemodynamic support.76–79 The intraprocedural differences are both morphological and pathophysiological: women tend to have smaller, more tortuous coronary arteries and therefore may require smaller DES, which are known to be associated with an increased risk of MACE.80 Furthermore, left main (LM) lesions in women are typically ostial (Figure 3) and do not need bifurcation stenting; however, they are more severely calcific and more commonly require the use of rotational atherectomy.78 The lower SYNTAX score calculated in women undergoing PCI of the LM is consistent with more frequent ostial involvement, but this alone fails to explain the trend towards worse outcomes.74 In fact, increased periprocedural MI rates and more frequent periprocedural bleeding in women treated with PCI than in women undergoing CABG have been reported in the EXCEL RCT and other studies.74,76,78
Concerning medical therapy and secondary prevention, antiplatelet therapy and statin prescriptions for women are less often optimised according to current guidelines, and women are less frequently referred to cardiac rehabilitation.76 Most studies agree on a higher risk factor burden, as well as increased rates of periprocedural complications and MACE, among women undergoing ULMCA PCI, although this is often mitigated after adjustment for confounders.74,78,79 The interaction between sex and revascularisation strategy shows favourable results for CABG, which appears to be associated with lower rates of death and MI among women, but these results are not sustained at long-term follow-up.59,74 Some recent registry data report comparable outcomes between PCI and CABG in women treated with new-generation DES.77 Of note, many studies suggest that further specific research is needed to determine optimal treatment modality in women with ULMCA disease.
Conclusion
The current findings build on prior studies on the potential differences in the pathobiology and natural history of coronary disease in women compared with men. Despite a lower atherosclerotic disease burden and reduced target lesion complexity, women remain at high risk of MACE after PCI, which underscores the need for the use of appropriate evidence-based therapies in this population. This apparent paradox also highlights the need for further investigation, because this may help elucidate why women may be at higher risk of ischaemia-driven target lesion revascularisation than men and whether there are any periprocedural or post-procedural interventions that could be undertaken to help improve outcomes.