Coronary spasm (CS) represents an important functional cardiac disorder, characterised by exaggerated vasoconstriction of the coronary arteries leading to transient myocardial ischaemia and anginal chest pain. Attilio Maseri’s work was pioneering in demonstrating the clinical relevance of CS as a functional vasomotor disorder, which is associated with an increased risk of non-fatal cardiovascular events and substantial morbidity due to impaired quality of life.1–3 CS may occur in epicardial coronary arteries and/or the coronary microvasculature.4 Diagnosis of CS can be confirmed by intracoronary provocation testing using either acetylcholine (ACh) or ergonovine (ER) as pharmacological stimuli.5,6
Differences regarding the prevalence and clinical presentation of CS have been suggested for patients of different ethnic backgrounds, especially in Asian compared with white individuals.7 Furthermore, different clinical and angiographic characteristics have been described in patients with non-obstructive coronary artery disease (CAD) and pathological ACh spasm test, revealing a preponderance of epicardial spasm in men, smokers and MI and non-obstructive coronary arteries (MINOCA) patients, as well as in patients with diffuse non-obstructive atherosclerosis. On the other hand, microvascular spasm occurs more frequently in women and in patients presenting with stable angina and diastolic dysfunction.8,9 This review will provide an overview on ethnic and sex differences in patients with CS.
Ethnic Differences
For a long time, ethnic differences regarding the prevalence and angiographic patterns of CS have been proposed. In fact, it was suggested by Maseri et al. that Asian patients have a higher frequency of CS and a more diffuse coronary hyper-reactivity, including multivessel spasm, compared with white patients.7 Subsequently, Maseri established an international collaborative research team comparing coronary reactivity in Japanese and white patients (15 Japanese and 19 Italian patients) 14 days after an acute MI. In establishing this prospectively conducted study, Maseri was insistent that “the same protocol needs to be undertaken in Japan and Italy” (two of the investigators supervised the protocol in both countries – ML Finocchiaro and J Beltrame) and that a “well-defined clinical study cohort is required” (patients with recent ST-elevation MI were included). In this study, the Japanese individuals exhibited greater coronary hyper-reactivity to ACh, with a twofold higher prevalence in a per-patient analysis (80% versus 37%) and a threefold higher prevalence in a per-artery analysis (47% versus 15%). The incidence of focal spasm in the per-segment analysis was 7% versus 2%, respectively. Furthermore, the Japanese cohort had a higher prevalence of multivessel spasm (64% versus 17%) and a greater constrictor response in coronary artery segments that did not fulfil the diagnostic criteria for coronary artery spasm.10
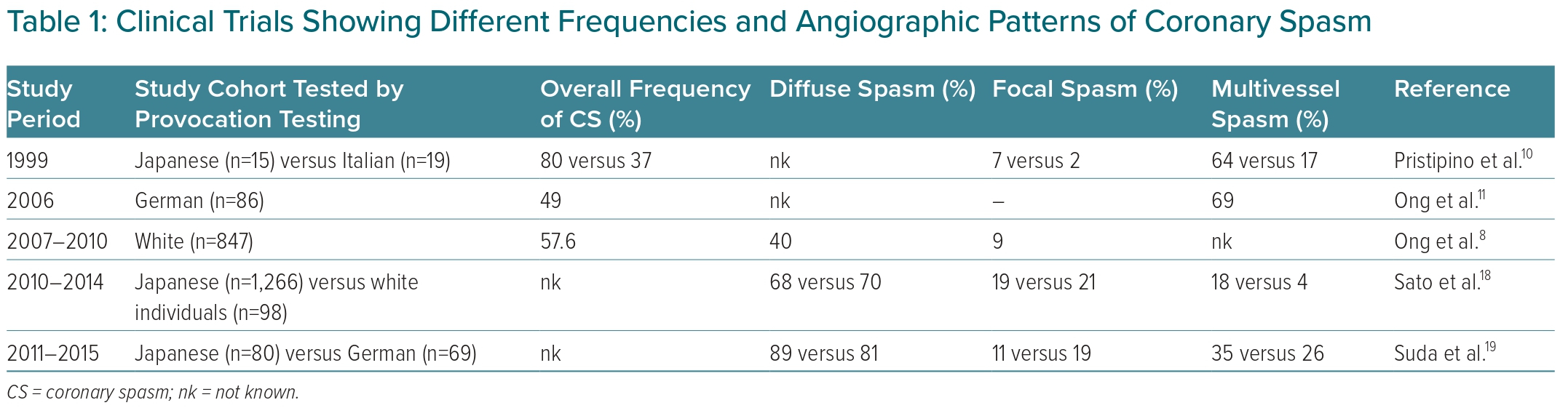
Although CS has been proposed to be more common in Asian countries, other studies have revealed that the prevalence of CS in white individuals may be higher than previously thought (see Table 1 for an overview). In a study by Ong et al., a cohort of German patients with suspected acute coronary syndrome (ACS) who underwent coronary angiography and showed no culprit lesion were investigated by ACh provocation testing.11 In 42 out of 86 patients (49%), CS was documented. In 16 patients, ACh provocation testing was performed in all three coronaries, in which multivessel spasm was found in 69%. Similar results were obtained in a subsequent trial assessing the clinical usefulness, angiographic characteristics and safety of intracoronary ACh provocation testing in white patients with unobstructed coronary arteries.8 Among 847 patients who underwent ACh testing, 488 were diagnosed with CS. Of these, 283 patients (33.4%) showed epicardial CS and 205 patients (24.2%) showed microvascular spasm. Epicardial spasm was most often diffuse (40%) and located in the distal parts of the epicardial vessels, whereas 9% of patients showed proximal and focal epicardial spasm. Although similar to the above prospective study, the prevalence of epicardial spasm in Japanese individuals does not appear to be as high in retrospective comparisons with large studies among white individuals.
Several characteristics, such as smoking, lipid metabolic disorders and gene expression, have been linked to the occurrence of CS. As the incidence of cigarette smoking in Japanese people is high, it was assumed by Miwa et al. that this might be one of the reasons why the prevalence of CS appears to be higher than in white individuals.12
Furthermore, some genetic variants associated with CS have been identified in Asian patients only, for example, aldehyde dehydrogenase 2 and Rho-associated kinase 2, whereas genetic polymorphisms within the endothelial NO synthase gene or polymorphisms within the endothelin-1 pathway have been identified in both Asian and white CS patients.13–15 Variations in the aldehyde dehydrogenase-2 genotype are present in 30–50% of Japanese, Korean and Chinese populations, but not within white or African populations. A deficiency in aldehyde dehydrogenase-2 that results in increased production of reactive aldehydes and oxidative stress was associated with CS in Japanese patients.16,17 Nevertheless, further investigations are necessary to elucidate the role of different genetic profiles for potential ethnic differences in CS.
Interesting results were obtained during a more recent study by Sato et al., in which the clinical characteristics and long-term prognosis of Japanese and white patients with a total of 1,457 patients (Japanese/white individuals, 1,339/118) suffering from vasospastic angina were analysed.18 Of these, 84% of white patients and 95% of Japanese patients underwent ACh testing to confirm the diagnosis. Importantly, there were no significant differences in both ethnic groups concerning the prevalence and patterns of CS, with two-thirds of the patients showing diffuse spasm (68% versus 70% in Japanese compared to white individuals) and around 20% exhibiting focal spasm (19% versus 21%, respectively) during ACh testing. However, multivessel spasm was documented more frequently in Japanese than in white individuals (18% versus 4%). Moreover, the survival rate after 5 years, free from major adverse cardiac events (MACEs), was slightly but significantly higher in Japanese than in white patients (86.7% versus 76.6%). Interestingly, the treatment strategy turned out to be different in the two ethnic groups, with a higher prescription rate of calcium channel blockers (CCBs) in Japanese patients (96% versus 86%), whereas nitrates (46% versus 59%), statins (43% versus 65%), renin-angiotensin system inhibitors (27% versus 51%) and β-blockers (10% versus 24%) were more commonly prescribed in white patients.
A recent study comparing German and Japanese patients with epicardial CS demonstrated even more similarities than differences in the angiographic patterns of CS.19 In this trial, 149 contemporary patients with resting angina and unobstructed coronary arteries with ACh-induced CS were enrolled between 2011 and 2015 in Stuttgart, Germany (n=69) and Sendai, Japan (n=80). Patients were analysed regarding type of spasm (focal/diffuse), dose of ACh leading to CS and frequency of multivessel spasm. The results of this study revealed diffuse spasm as the most prevalent type of spasm (85%), whereas 15% of patients showed focal spasm. Multivessel spasm was found in 31% of patients. The distribution of focal and diffuse spasm types was comparable in both Japanese and German patients (89% versus 81% and 11% versus 19%, respectively). Moreover, for both spasm types, no significant differences were observed regarding the ACh dose required to induce spasm when Japanese patients were compared with German patients. Interestingly, the frequency of multivessel spasm was similar in both ethnic groups (35% versus 26%), showing no statistically significant differences.
This was different to previous results, where a more than fourfold higher frequency of multivessel spasm patients was shown for Japanese patients.18 The authors speculated that discrepancies in the rates of multivessel spasm might be explained by differences in study protocols and data analysis. For example, in Asian countries ACh testing of the right coronary artery (RCA) is more regularly performed (with insertion of a backup pacemaker) compared with other countries.10,18 As a consequence, the rate of multivessel spasm might be higher in Japanese patients.
In the aforementioned study by Suda et al., only patients with epicardial spasm provoked in the left coronary artery (LCA) were included for analysis in the Japanese and German groups. This might explain the similar frequencies of multivessel spam seen in both ethnic groups, which is in contrast to previous studies. In addition, Sato et al. also included ER as a pharmacological agent for provocation testing during coronary angiography, whereas Suda et al. did not. As ER and ACh act through different receptors (serotonergic receptors versus muscarinic cholinergic receptors, respectively), these different stimuli may cause different vasomotor responses. Indeed, ER testing is known to rather provoke focal and proximal spasms, whereas provoked spasms by ACh appear to be more diffuse and distal,19 a fact that might explain the high rates of diffuse spasms in previous studies.
Nevertheless, provocation testing with either ACh or ER is broadly applied in daily clinical use in Asia, particularly in Japan, whereas spasm provocation testing is not as well established in clinical routine in Europe and the US, although it has been proven to be useful and safe.8,20,21
The differences in findings between these ethnic comparisons in CS (summarised in Table 1) may reflect differences in:
- study design: a prospective, controlled trial versus retrospective analyses;
- study cohort: acute MI patients versus those with stable angina and non-obstructive coronary arteries;
- CS risk factor differences;
- choice of provocation agent; and
- provocation protocol.
Thus, further epidemiological and pathophysiological studies are needed to determine the role of CS in different ethnic populations.
Sex Differences
CS Prevalence, Patient Characteristics and Prognostic Factors
As early as 1980, clinical observations by Maseri and colleagues indicated a predominance of female patients presenting with spontaneous anginal attacks and prior or ongoing myocardial ischaemia despite angiographically normal coronary arteries, while stenosis >75% relating to at least one vessel was more prevalent in male patients. Even then, the authors suspected that CS was an important cause of angina, in particular in young female patients without visible coronary stenosis, in whom coronary vessels appear to be more prone to abnormal vasomotion.22 Decades later, these observations could be confirmed by evidence from large clinical studies revealing that in patients with anginal chest pain undergoing coronary angiography for suspected CAD, normal arteriograms or non-significant coronary stenoses (<50% stenosis) were more frequent in female (60–70%) than in male (about 30%) patients.23–25
The main reason for the significantly lower prevalence of obstructive CAD in women is in part due to the protective effects of female sex hormones on the development of CAD, which decreases after the onset of menopause to approach a prevalence comparable to that of men, with a delay of approximately one decade. Besides the protective properties of female sex hormones on the one hand, the vessels of women are naturally much more exposed to varying hormonal influences on the other hand, which may favour a more distinctive vascular reactivity through indirect mechanisms or direct interaction with vascular cells, including endothelial as well as smooth muscle cells. Hence, the absence of relevant flow-limiting epicardial stenoses does not exclude the presence of an abnormal coronary vasomotion in response to vasoactive substances such as ACh.26,27
Above all, it has been shown that these patients suffer more frequently from chronic pain disorders compared to patients with obstructive CAD (23% versus 10%; p<0.001), reinforcing the need for a confirmed diagnosis and appropriate therapy.25 Thus, a large European study involving 1,379 consecutive patients with stable angina and unobstructed coronary arteries (no epicardial stenosis >50% by visual assessment) undergoing ACh provocation testing for assessment of epicardial and/or microvascular spasm revealed that pathological test results were more common in females (70% versus 43%; p<0.001).28 In particular, microvascular spasm was significantly more prevalent in women (42% versus 20%; p<0.001), whereas epicardial spasm occurred only slightly more frequently in female compared to male patients (28% versus 23%; p<0.05).28
A significantly more frequent pathological ACh test result in women in the setting of unobstructed coronary arteries could also be confirmed in further clinical studies by Ong et al.8,29 Accordingly, in Japan microvascular spasm also appears to be diagnosed significantly more often in women (21% versus 3%; p<0.0001) presenting with non-obstructive coronary arteries (<50% diameter), whereas epicardial spasm is more common in men (70% versus 49%).30
The observed discrepancy regarding the sex-specific distribution of epicardial and microvascular spasm between the European and Japanese study populations is likely due to the different diagnostic criteria used in these studies. Thus, beyond the standardised COVADIS (Coronary Vasomotion Disorders International Study Group) diagnostic criteria for microvascular spasm, defined as reproduction of the usual chest pain and ischaemic ECG changes without significant epicardial spasm, this Japanese study also required an increase in cardiac lactate production and a decrease in coronary blood flow to qualify for a microvascular spasm diagnosis.31 Furthermore, different ACh doses (20–100 µg in the Japanese versus 2–200 µg in the European study) and cut-off values for diameter reduction defined as epicardial spasm were used (>90% in the Japanese versus >75% in the European study). Nevertheless, a preponderance of epicardial spasm in male and microvascular spasm in female patients with myocardial ischaemia and non-obstructive CAD was also confirmed by Montone et al.9
Regarding epicardial spasm subtypes, several Japanese studies revealed that diffuse vasoconstriction occurred more frequently in women, and focal spasm was observed more frequently in male patients.32–34 However, it should be considered that patients with obstructive CAD were also included in these studies. Thus, previous studies have already shown that focal spasm is related to the presence of visible atherosclerotic alterations of the vessel wall, such as intima-media thickening and increased plaque burden at sites of focal spasm.35–38 Sato et al. demonstrated that severe epicardial stenosis (≥75%) was significantly more prevalent in the focal compared with the diffuse spasm group (33% versus 17%; p<0.001), which, as expected, was associated with a worse long-term prognosis than diffuse spasm.33 Moreover, in patients with epicardial CS the predictor of MACE appears to be different between men and women. Age and electrical abnormalities, including ventricular tachycardia and VF, were more associated with female sex, whereas structural abnormalities, including coronary stenosis and previous MI, were associated with male sex.39
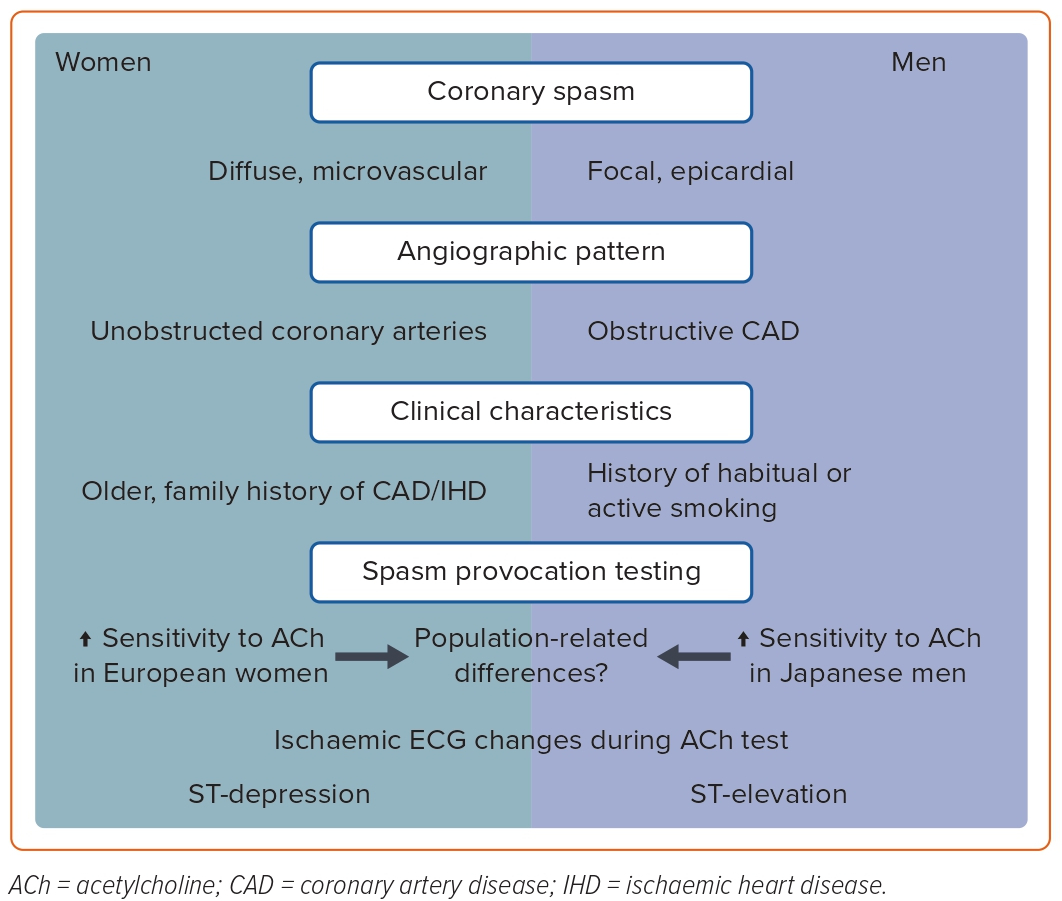
Concerning traditional cardiovascular risk factors, both European and Japanese studies revealed that female CS patients were significantly older and more likely to have a family history of cardiovascular/ischaemic heart disease. However, compared with male patients, a significantly lower proportion of women were active smokers or had a history of habitual smoking (see also Figure 1). Apart from the finding by Aziz et al. that women in the study had a higher prevalence of hypertension, there were no conspicuous gender differences in other cardiovascular risk factors or duration and type of symptoms.28,29,34,39
Medication and Clinical Outcome
In female and male patients with epicardial CS, CCBs (a first-line agent in CS therapy) were prescribed with comparable frequency, whereas the use of dihydropyridine-type CCBs was significantly higher in male patients.28,34,39 Furthermore, in a study by Sueda et al. the prescription rate of aspirin and nitrates was significantly higher in male patients. Moreover, in a study by Kawana et al. the use of antiplatelet agents was significantly higher in male patients (50% versus 38%; p<0.001), while statins were taken slightly but significantly more often by women (37% versus 32%; p=0.049).
Regarding the administration of β-blockers, angiotensin receptor blockers or angiotensin-converting enzyme inhibitors, no gender-specific differences were found.34,39 During continued guideline-based medical therapy with a low rate of dose reduction/discontinuation (2% in male versus 1.6% in female patients; p=0.63) within the follow-up period, both clinical outcomes (primary endpoint: MACE; secondary endpoint: all-cause death) and the overall 5-year MACE-free survival rate (94% versus 93%) were comparable between male and female epicardial CS patients.39
Sueda et al. consistently confirmed no prognostic differences regarding sudden cardiac death- and ACS-free survival rates within the follow-up period of 80 months between both sexes with ACh-provoked epicardial spasm.34 Importantly, it should be considered that in these studies epicardial CS patients with obstructive CAD were also included. Moreover, Kawana et al. noted that the long-term prognosis for MACE-free survival rate among Japanese women <50 years of age was significantly lower (<50 years: 82% versus 50–64 years: 92% versus ≥65 years: 96%; p<0.01). The authors attributed this finding primarily to the high prevalence of smoking in the female group <50 years (<50 years: 54% versus 50–64 years: 24% versus ≥65 years: 13%; p<0.001), which is an important known risk factor for CAD as well as CS. A strong association between cigarette smoking and CS has already been reported in premenopausal women.40
Sex Differences during Spasm Provocation Testing
Aziz et al. provided the first clinical evidence of increased sensitivity to ACh in female patients requiring a lower ACh dose (incremental doses of 2, 20, 100 and 200 µg) to elicit a pathologic test result, which was most evident at ACh doses of 20 and 100 µg infused into the LCA.28 In contrast, a recent study by Sueda et al. could not confirm significant sex-dependent differences regarding the frequency of maximum ACh dose provoking a pathological response by incremental administration of 10, 20, 50, 100 and 200 µg into the LCA and 10, 20, 50 and 80 µg into the RCA. However, if the mean maximum used ACh dose was compared, female patients showed a pathological test result in both the LCA (104 ± 52 µg versus 91 ± 50 µg; p=0.012) and RCA (59 ± 21 µg versus 54 ± 23 µg; p=0.042) at a significantly higher ACh dose. Likewise, in the subgroup of patients without obstructive coronary arteries, female patients also showed a higher mean maximum used ACh dose provoking CS in both the LCA and RCA compared with male patients (110 ± 52 versus 91 ± 50; p=0.012).34 These findings suggest population-related differences relating to ACh sensitivity between men and women (Figure 1). However, divergent definitions of a pathological test result as well as procedural differences limit the comparability of these studies. In contrast to Sueda et al., in the study by Aziz et al. a pathological test result included both epicardial and microvascular spasm, while in the study by Sueda et al. both LCA and RCA reactivity to ACh were examined by default.28,34 Further studies are needed to clarify this issue.
Interestingly, comparison of ischaemic ECG changes during ACh provocation testing revealed that ST-depression was recorded more frequently in female patients, whereas ST-elevation was observed more frequently in male patients. This observation could also be confirmed in the subgroup of female patients without obstructive CAD.34 In line with these findings, Kawana et al. documented that ST-depression occurred more frequently in female and ST-elevation more frequently in male epicardial CS patients during spontaneous angina attacks (Figure 1).39
Regarding the occurrence of complications during coronary reactivity testing, it has been previously reported that ventricular tachycardia or VF were significantly more prevalent in female patients during spasm provocation testing with ACh and/or ER (5% versus 3%; p=0.02).39 However, recent studies in which provocation testing was performed with ACh alone exhibited a low complication rate that was comparable in both sexes.21,28,34
Sex-Specific Differences and Clinical Implications
Despite the fact that male and female patients report their symptoms differently, clinical history alone can often not distinguish between obstructive CAD and CS.41 Thus, in patients undergoing invasive coronary angiography where unobstructed epicardial arteries are found, further diagnostic methods to determine the diagnosis are warranted. This comprises – among others – intracoronary provocation testing in search of CS. In particular, microvascular spasm seems to be more prevalent in female patients suffering from anginal chest pain despite angiographically unobstructed coronary arteries. Since the vasoconstrictor component only comprised one component of coronary microvascular dysfunction, the (co)existence of vasodilator dysfunction of the coronary microvasculature, which is associated with a significantly higher prevalence in female patients, should also be considered in the diagnosis and treatment of potential CS.42 Further large-scale studies are warranted to provide targeted sex-specific treatment recommendations for CS patients.
Conclusion
There is heterogeneity in the findings of coronary vasomotor reactivity studies comparing Japanese and white patients. However, recent clinical data suggest that many of the differences can be attributed to varying procedural approaches and patient selection in Asia and Europe. Furthermore, apparent differences may also be explained by different genetic variation profiles associated with CS within Asian and white populations. Nevertheless, regardless of ethnicity, there is considerable evidence for consideration of diagnostic and prognostic differences in male and female CS patients (summarised in Figure 1) for appropriate management of patients with CS. 










