In the Cardiology Masters section of European Cardiology Review, we bring you an insight into the career of a key contributor to the field of cardiology.
In this edition, we feature Dr Patrick Serruys, professor of cardiology at the National Heart and Lung Institute at Imperial College, London, UK.
The hippopotamus and left ventricular contractility
In 1947, shortly after my birth, my family arrived in Zaire, now the Democratic Republic of Congo (DRC), in Africa. It was in the postwar period, and my parents had no choice other than to emigrate. So, my youth (until my return to Belgium) was in Africa – an experience of living in wide open space under the African sun, with wild animals all around. There were no seasons; it was a great feeling of liberty in an unbelievable continent with unlimited space and extraordinary wildlife.
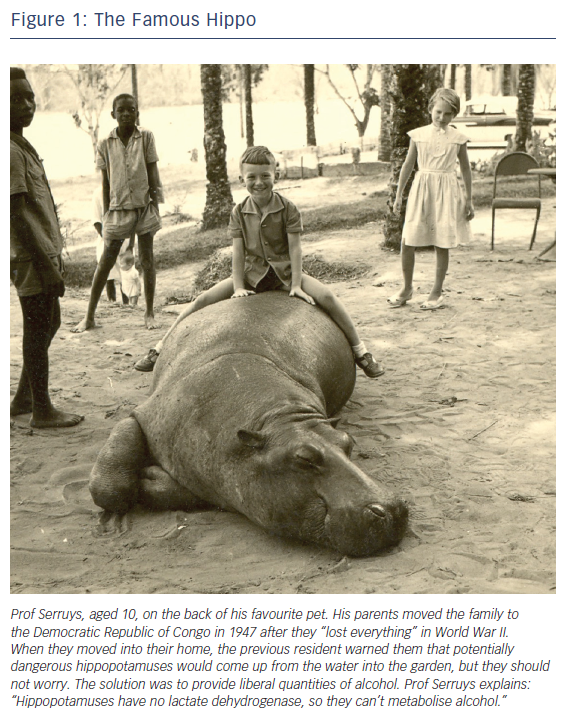
It has been published in Circulation that my favourite pet was an alcoholic hippopotamus – there are pictures of it (Figure 1).1 We lived in a house that had gardens that ran down to the Congo River and, when we moved in, the previous resident told my father that a potentially dangerous hippopotamus would come up from the water into the garden, but we should not worry.
The solution – in an age when animal welfare was little developed and it was politically correct to give alcohol to animals – was to provide liberal quantities of alcohol. Vermouth was the preferred alcohol and, because the animal has no lactate dehydrogenase to metabolise the alcohol, he would fall asleep, not to say that he was in a coma. Then, with my friends, I used to climb on his back, open his eyes, open his mouth, look in his ears.
That hippopotamus became famous when my mentor showed those pictures to Edmund Sonnenblick, a great expert on left ventricular contractility. At the time, the concept was described as a ‘white elephant’, because it was very difficult to catch and to comprehend. There were multiple diseases that could contribute, and a lot of debate on a definition. One day, I was in a debate with Sonnenblick. I was still a very young man, and that’s how my mentor, Prof Paul Hugenholtz, presented me to the audience: he said this young fellow was not afraid to debate with a great expert. He quipped that, instead of chasing the white elephant, I was able to master the black hippopotamus.
Leaving Socrates behind
I spent six years studying Greek and Latin – at the end of high school, I was more fluent in these languages than I was in French, German, English or Flemish. When the time came to make a decision about future studies, I wrote a letter to my father saying that I wanted to study pure philosophy. My father wrote back to me from the DRC, saying: “Boy, this is fine, but it will be difficult being Socrates in the 20th century. You are a good student, so why don’t you do something like engineering, medicine or law, as well as philosophy?”
So I entered the University of Leuven to study philosophy in parallel with medicine. My plan at the time was to combine philosophy with psychiatry but, after one year, I gave up on the philosophy. The course was boring, with a lot to memorise and it was all about old stuff. I was 17 and very existential at the time.
Then, in the second year of studying medicine, I joined the department of physiology run by Xavier Auber. I became fascinated by the physiology of the vascular system – in particular, the contraction of smooth muscle and the contraction of mammalian and amphibian muscles. In Prof Auber’s laboratory, I studied contraction of the sartorius muscle of the frog, and spent a lot of time on the force–velocity relationship.
Then I joined Prof Alan Hodgkin, later Sir Alan; he won the Nobel Prize in 1963 with Andrew Huxley and John Eccles for their discoveries concerning the ionic mechanism involved in excitation and inhibition of the peripheral and central portion of the nerve-cell membrane. I was based at the Marine Institute, Marine Biological Association in Plymouth, England, which was a wonderful experience, studying the voltage clamp technique. During the day, we would fish for squid, which have giant axons and nerve-cell membranes and, at night, we were using the Hodgkin’s voltage-clamp technique to investigate nerve transmission in the squid’s huge nerve fibre. However, I soon realised that physiologists were exceptional individuals, with knowledge of biochemistry, physiology, statistics and engineering; Aubert had made his own strain gauge. For me, I wanted to focus on being just one thing, and that was why I decided to join the clinical field.
Setting out on the path
In my final year of cardiology training at the University of Leuven, I happened to attend a meeting on the use of computers in cardiology and met Prof Paul Hugenholtz, who asked me to visit the thoracic centre, and I fell in love with the place immediately.
He was an extraordinary mentor, the father of the European Society of Cardiology, and gave me full confidence, which really shaped my personality, with the classic motto “Nothing is impossible”. When I graduated summa cum laude in internal medicine in 1972, I continued to work on muscle physiology using a creatine phosphokinase block.
During my first years in cardiology, 1973–7, we were basically making diagnoses for the surgeon – providing fresh flesh to them, as Hugenholz put it. In our institution, we were the great provider of coronary bypass and valve replacement surgery. I had just got married and my wife suggested I should spend more time at home so, in 1974, I started working in the cath lab in Leuven, as it was a more elective, planned way of life, and I fell in love with this sort of working environment. This was before the advent of interventional cardiology as we know it. When the angioplasty era came, we jumped on the opportunity to become a treating physician independent of the surgeon.
Developing the field of interventional cardiology
Very soon, I became aware of restenosis occurring after balloon angioplasty. For many years, I investigated multiple pharmacological treatments – ketanserin, angiotensin-converting-enzyme inhibitors, anti-sense therapy – and all studies were published in the New England Journal of Medicine and The Lancet. There were 13 unsuccessful trials in total; I felt like the champion of the negative trial.
But during this period, through to the early 1980s, I established the methodology of quantitative coronary angiography with the bioengineering group at the Thoraxcenter in Rotterdam. In those days, I also developed my worldwide network with experts to unravel the issue of restenosis. After the unsuccessful pharmacological trials, I shifted my focus to mechanical device engineering such as stenting and, in 1986, introduced the technique in the Netherlands.
The advent of the drug-eluting stent
The bare-metal stent was creating even more new intimal hyperplasia than balloon angioplasty, and then I discovered – albeit by chance – the concept of the drug-eluting stent. At the Cordis Corporation facilities in New Jersey, I jumped on the concept, using the latest scientific and experimental knowledge in the field of molecular biology of neointimal inhibition. Eduardo Sousa, in São Paolo, Brazil, and I introduced the drug-eluting stent for the first time to the world in 1999.
This was a revolution for interventional cardiology, as it drastically reduced the restenosis rate after an intervention; however, implantation of a permanent metallic prosthesis was viewed as a major drawback in the treatment of coronary artery stenosis. Therefore, in 2006, I introduced with John Ormiston, of Mercy Hospital, Auckland, New Zealand, the worldwide use of fully biodegradable, drug-eluting scaffolds that eliminated the presence of a permanent metallic foreign body in the coronary circulation.
I am proud that, in the implementation design of quantitative coronary angiography, the initial algorithm I developed with Hans Reiber at the Thoraxcenter in Rotterdam remains unchanged and the gold standard 40 years after its inception. And, of course, of the value demonstrated by the bare-metal stent, the drug-eluting stent, and the introduction of the PLLA bio-resorbable scaffold.
Reaping the rewards
I have received many awards; my office is full of diplomas and medals, but the TCT Career Achievement Award in 1996 has a special place in my heart and in my memories, because TCT director Dr Marty Leon flew my entire family – my parents, wife and the three kids – to Washington for the event. When I went to stage to thank him for bestowing this honour on me, I suddenly realised in a kind of extraordinary emotional shock that my entire family was in the main arena watching the whole ceremony.
The second moment that stands out was a standing ovation at the American Heart Association in November 2001, two months after the terrible events of September 2001. There was a gloomy atmosphere and a metal gate at the entrance of the main arena, but my speech was full of enthusiasm, optimism and novelty in the field of cardiology, which is probably what triggered a standing ovation. First, I thought that it was a manifestation of some individual action – but then I thought perhaps that if only the people on my right were standing up, it was because there was a leak in the plumbing and they’d just realised their feet were in water. It was only when I saw the Dutch attendees standing up that I realised it was a standing ovation.
Finally, I received a career achievement award from the American College of Cardiology, as well as the gold medal of the European Society of Cardiology. I received the latter jointly with Dr Pedro Brugada – we both became professors of cardiology in 1988 – and it was a huge ceremony in a big cathedral. There were no slides; from behind the lectern it felt rather like talking as a priest.
In terms of my work, I have good memories of the first streptokinase intracoronary, the first bare metal stent, the first drug-eluting stent and the first valve implantation. Those are things that you cannot forget.
Reflecting on the future
I think future of cardiology will turn out to be, as usual, unexpected. Over my career, I’ve constantly been surprised by the direction it has taken. There has been tremendous competition between device and pharma over the past 50 years and I am sure that nanotechnology, gene therapies and artificial intelligence will play a major role in the future. By 2025, computers will have the capacity of the human brain; big data is coming very quickly, and advances in imaging and holograms will quickly appear and lead to a rapid pace of change in our practice.
I would tell others that the first step when you try to introduce something new is to be aware that medicine is terribly difficult and has immense ethical issues.
I will never forget the extraordinary dialogue with the patient that precedes the first in man. The patient must trust you. It is a frightening moral responsibility for you, when you treat the first patient, the first 10, the first 1,000 – before finally you have millions of people benefiting from something that you have introduced, such as a stent, a drug-eluting stent or a valve.
It is important to be curious. Don’t look at the past – try to guess the future. Be open to novelty. Keep thinking that, at the very end, whatever the discovery is, it has to be potentially beneficial to your father, your brother, your mother and your sister, and to basically every patient around the world.