Background
Alcohol is the most frequently consumed toxic substance in the world. Globally, one in three people drink alcohol, including 25% of women and 39% of men, and in Europe, up to 50% of adults consume alcohol regularly. On average, women consume 0.73 alcoholic drinks and men 1.7 drinks each day.1
Alcohol has a complex association with health, in particular cardiovascular health. Alcohol use is considered a leading risk factor for disease, and consumption is linked to more than 60 acute and chronic diseases.2 Whereas chronic excessive alcohol consumption is associated with decreased myocardial contractility, hypertension, cerebrovascular accidents, arrhythmias such as AF and MI, leading to progressive cardiac dysfunction and heart failure, low levels of alcohol consumption are perceived to have protective effects against ischaemic heart disease and diabetes.3–5
In contrast, health conditions with a clearly established correlation to alcohol intake, such as liver cirrhosis, show a linear relationship with alcohol use, with a clear dose-dependent increase in risk, even with one daily drink.6
In this review, we aim to clarify the current understanding of the impact of alcohol consumption on the heart and assess whether the claims of alcohol’s protective effects on the heart are valid.
Purported Beneficial Effects of Alcohol on the Heart with Low to Moderate Consumption
Although the purported beneficial effects of alcohol on the heart are not validated, there is nonetheless some literature regarding the reduced risk of cardiovascular diseases such as stroke, heart failure, MI and coronary artery disease with low to moderate alcohol intake (5–30 g/day).7,8 The lower risk of cardiovascular disease seen with low-to-moderate alcohol use is thought to be due to a combination of factors, including increased circulation of HDL and increased insulin sensitivity, as well as reduced oxidative stress, blood pressure, clotting factors and inflammatory markers.9
HDL has the most significant role in this reported cardioprotective effect; alcohol upregulates expression of the main apolipoproteins (A1 and A2) that compose HDL, which is inversely correlated with the development of atherosclerosis.10 Platelet function is also modulated favourably with alcohol use. Moderate alcohol intake has an antithrombotic effect by inhibiting the function of thromboxane A2, which is key in the activation of platelet aggregation.11 In addition, a meta-analysis showed that moderate alcohol consumption reduces plasma fibrinogen concentrations.12,13 Fibrinogen is converted into fibrin (via the action of thrombin) to create fibrin clots. Thus, the reduction of plasma fibrinogen concentrations and platelet aggregation theoretically lowers the risk of thrombotic events, such as MI and stroke.
Moderate alcohol intake has also been linked to increased insulin sensitivity due to increased adiponectin. Mouse models have shown that increased adiponectin can protect against ischaemia and cardiomyopathy.14,15 Adiponectin also plays a similar role to HDL in the prevention of the formation of foam cells by inhibiting platelet aggregation and macrophage activity.16
Detrimental Effects of Chronic Alcohol Consumption on the Heart
Despite enticing evidence for the benefits of low-to-moderate alcohol consumption on the heart, there are several well-defined detrimental effects of heavy alcohol consumption on the cardiovascular system. Chronic alcohol consumption is associated with an increased risk of cardiovascular disease via mechanisms such as decreased myocardial contractility, hypertension, arrhythmias, MI and, most notably, the development of alcoholic dilated cardiomyopathy (A-DCM).17
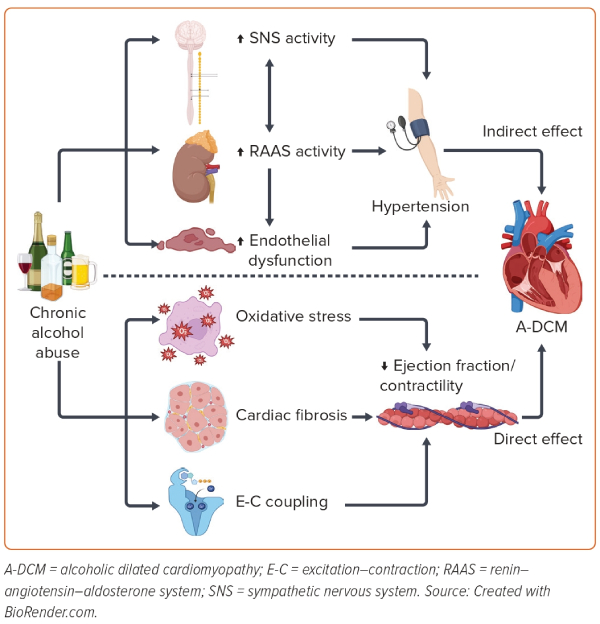
Several mechanisms, both direct and indirect, contribute to the myocardial dysfunction observed in excessive alcohol intake and A-DCM (Figure 1). Excess alcohol intake indirectly raises blood pressure via activation of the neurohormonal axis, the sympathetic nervous system and the renin–angiotensin–aldosterone system, and by promoting endothelial dysfunction.18 The toxic effects of ethanol and its metabolites lead to direct insult on cardiomyocyte contractility via oxidative stress, cardiac fibrosis and excitation–contraction coupling dysfunction.18
It is noteworthy that alcohol consumption has been linked to both a reduction and an increase in oxidative stress. This apparent dichotomy highlights that the effects of alcohol on oxidative stress are complex and can vary depending on factors such as the type and amount of alcohol consumed, the time frame over which it is consumed and individual differences in metabolism. Some studies have shown that certain compounds found in alcoholic beverages, such as polyphenols and resveratrol in, for example, red wine, have antioxidant properties and can scavenge free radicals, which are reactive molecules that can cause oxidative damage to cells.19 These compounds may help reduce oxidative stress and its associated negative effects on the body. It is believed that high levels of alcohol intake generate more free radicals, which overwhelms the body’s antioxidant defences and ultimately leads to increased oxidative stress.19
Alcoholic Dilated Cardiomyopathy
A-DCM is defined as a form of dilated cardiomyopathy secondary to heavy and longstanding alcohol misuse. It is recognised as its own clinical entity in the ICD-10, but remains a diagnosis of exclusion because it is not possible to differentiate it clinically or histologically from idiopathic dilated cardiomyopathy. Hence, the history and amount of alcohol intake is pertinent to diagnosis.
Acute Effects of Alcohol Consumption
In 1978, a seasonal peak incidence of arrhythmias around the year-end holiday period was found, which corresponded with episodes of binge drinking and peak alcohol sales. The phenomenon of ‘holiday heart syndrome’ was coined for patients who experienced arrhythmias after episodes of binge drinking, characterised by an acute cardiac rhythm and/or conduction disturbance associated with heavy ethanol consumption in a person without other clinical evidence of heart disease and the arrhythmia disappearing with abstinence.20
Short-term alcohol consumption has also been linked to hypotension during orthostatic stress secondary to both impairment of vasoconstriction and a blunting and latency of muscle sympathetic nerve activity.21,22 In a double-blind randomised controlled trial, Narkiewicz et al. demonstrated that alcohol induces orthostatic hypotension in young, healthy subjects by simulating cardiopulmonary reflex vasoconstriction on standing, using lower body negative pressure.21 Narkiewicz et al. found that alcohol results in a twofold increase in the hypotensive response to marked orthostatic response within 40 minutes of consumption.21 Carter et al. confirmed that short-term alcohol consumption both reduces arterial blood pressure responsiveness to orthostatic challenges and raises resting heart rate.22 Combined, these phenomena may be the primary factors in presyncope and syncope related to alcohol consumption.
In patients with congestive cardiac failure, short-term alcohol intake has been shown to reduce arterial blood pressure.23 Furthermore, recent work has crystallised this dynamic interplay between the heart and arterial vessels. Galati et al. have shown an active compensatory vascular role, a reduction in all measured vascular kinetic parameters, consistently across patients with three groups of heart failure (heart failure with reduced ejection fraction [HFrEF], heart failure with moderately reduced ejection fraction and heart failure with preserved ejection fraction [HFpEF]), establishing the clear interplay of the heart and its tributary peripheral vessels.24
Longer-term Effects of Alcohol Consumption
It remains unclear what amount of alcohol ingestion, and over what period, is required to develop A-DCM. The consensus, based on extrapolations of case-control studies, seems to be that alcohol ingestion of >60–80 g/day for 5 years is likely to be contributory. A meta-analysis of 84 studies showed that alcohol consumption of 2.5–14.9 g/day, compared with abstaining, showed a 14–25% risk reduction for cardiovascular disease mortality, coronary heart disease mortality, stroke mortality and incidence of coronary heart disease and stroke events.4 For coronary heart disease outcomes, all levels of alcohol intake >2.5 g/day had a similar degree of reduction.4 For cardiovascular disease and stroke mortality, the dose–response relationship was less clear and consistent with a J-shaped curve, suggesting increased risk only with heavier alcohol consumption.4
A recent meta-analysis of alcohol intake and heart failure dose–response showed that a consumption of seven drinks per week was associated with a 17% lower risk of heart failure compared with abstinence.25 In that study, a non-linear J-shaped association was observed between consumption and the risk of heart failure and, compared with non-drinkers, and the RRs of heart failure across levels of alcohol consumption were 0.90 for three drinks/week, 0.83 for seven drinks/week, 0.90 for 14 drinks/week and 1.07 for 21 drinks/week.25
Epidemiology
Epidemiologically, higher levels of alcohol consumption have consistently been associated with subclinical measures suggestive of adverse left ventricular remodelling, such as increased left ventricular mass and left ventricular eccentric remodelling.26–28 The largest cohort study of more than 49,000 patients undergoing echocardiograms showed that higher levels of alcohol intake were associated with impaired diastolic function and increased left ventricular mass.27 Nakatani et al. demonstrated a dose-dependent impairment of diastolic functions, such as longer isovolumetric relaxation time, longer deceleration time, higher longitudinal atrial tissue Doppler velocity and lower mitral inflow E/A ratio, with longer drinking duration, compared with controls.29 Similar observations have since been reported using speckle tracking technology in other studies.29–31
Despite this evidence linking high alcohol consumption to subclinical adverse cardiac remodelling and impaired diastolic function by echocardiograms, longitudinal community-based studies have reported paradoxically lowered risk of heart failure with low–moderate alcohol consumption compared with no use.17,32–36 This paradoxical J-shaped association between heart failure and alcohol suggests that other risk factors are equally important in the equation. A recent Mendelian randomisation study concluded that genetically predicted alcohol consumption was not associated with greater risks of heart failure, in contrast with clearly documented increases in risks of stroke and AF, further supporting the theory that alcohol is not frequently the cause of cardiomyopathy and heart failure in the community.37
Women and Alcoholic Dilated Cardiomyopathy
On a population level, women tend to drink less alcohol than men, which could explain, in part, why women are often underrepresented in A-DCM studies.1 Decades ago, cross-sectional studies that estimated the frequency of A-DCM among individuals with a diagnosis of idiopathic dilated cardiomyopathy simply excluded women.38–40 In 2019, Mogos et al. estimated that the prevalence of new or existing A-DCM was 68 per 100,000, with a greater percentage of men than women (with a ratio of 8:1).41 In addition, recent studies have suggested that women tolerate a lower total lifetime dose of ethanol than men.42 Mogos et al. also studied differences in the incidence and distribution of co-occurring conditions among men and women with A-DCM and found that women were more likely to have co-occurring anaemia, thyroid disease and HFpEF.41 This underrepresentation of women in trials and the literature is well-recognised, and a recent review of the management of diabetes, heart failure management and women suggests that this leads to underestimation of cardiovascular risk and reduced therapeutic inertia, which contribute to the poorer prognosis of women with A-DCM.43
Management of Alcoholic Dilated Cardiomyopathy
Abstinence and reduction of alcohol ingestion have both been identified as effective management options in the treatment of A-DCM, but it remains unclear whether abstinence is better than reduction. A prospective study in 2018 with an 82-month follow-up period has recognised that both abstinence and reduction in alcohol intake contribute positively to left ventricular ejection fraction (LVEF) recovery.44
Interestingly, Guzzo-Merello et al. found that there was no statistically significant difference between abstainers and those reducing intake to a moderate level in transplant-free survival and LVEF improvement.45 However, a more recent study from 2022 has shown that abstinence led to statistically significant LVEF improvement compared with moderate drinking.46 Despite this, complete alcohol abstinence has remained the recommendation because it is considered that maintaining mild–moderate alcohol intake is difficult, with a high risk of relapsing to heavy alcohol use. To encourage and maintain abstinence, a combination approach using pharmacological and psychological therapies should be employed.
The pharmacological treatment for alcoholic cardiomyopathy remains unchanged from the gold-standard four-pillar approach to HFrEF management, namely angiotensin receptor–neprilysin inhibitor, β-blockers, sodium–glucose cotransporter 2 inhibitors and mineralocorticoid receptor antagonists. However, if device therapy (cardiac resynchronisation therapy and ICD) is considered in HFrEF management, it is important to carefully assess suitability for implantation, wound and device care compliance, adherence to follow up and the possibility of ICD therapy due to electrolyte imbalance due to ongoing alcohol abuse. Conventionally, patients with HFrEF whose symptoms remain refractory to treatment are considered for cardiac transplantation. However, in most transplant services, any alcohol and/or substance misuse remains an absolute contraindication to transplant, and there are very few reported cases of patients with alcoholic cardiomyopathy receiving heart transplants. In a series of 94 patients with excessive chronic alcohol consumption with A-DCM, only 15% achieved heart transplantation.45
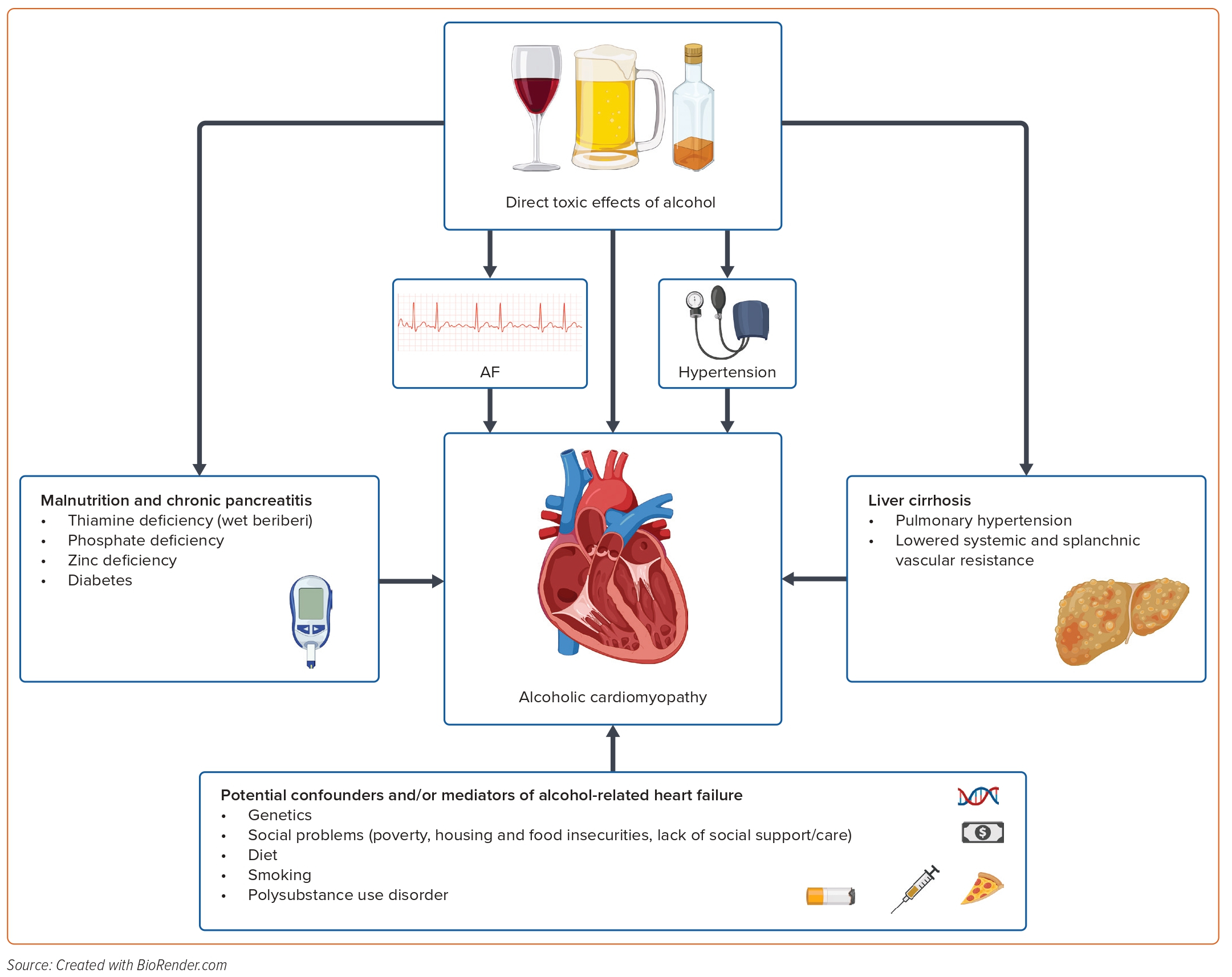
Furthermore, an individualised and holistic care plan should be used in the treatment of A-DCM, including a strong emphasis on psychological counselling and support. The clinician should consider and treat alcohol-induced damage such as liver cirrhosis, malnutrition and electrolyte disturbances, which also contribute to cardiac abnormalities. Other considerations include dietary changes with a view to reducing sodium and sugar intake and/or changing to a Mediterranean diet, which is effective in the prevention of cardiovascular events in patients with A-DCM.47 Other lifestyle measures to control risk factors contributing to cardiac disease, such as smoking cessation, managing hypertension and diabetes and stopping recreational drug use, will aid in improving cardiac function in patients with A-DCM.48
Clinical Correlates
Several mechanisms have been hypothesised to underlie the diagnosis of alcoholic cardiomyopathy (Figure 2), and the interaction between alcohol consumption and other risk factors, such as socioeconomic factors and genetics, is not well established. In addition, the amount of alcohol ingested per sitting also seems to play a role in the mechanism that underlies the diagnosis of A-DCM. A trial that mimicked binge drinking by ingesting a set amount of alcohol in 3–4 hours showed acute, reversible changes in the myocardium with evidence of inflammation on cardiac MRI.49 Furthermore, autopsy reports of patients with chronic alcohol use have shown increased epicardial fat, endocardial fibrosis and iron deposition in the myocardium.50
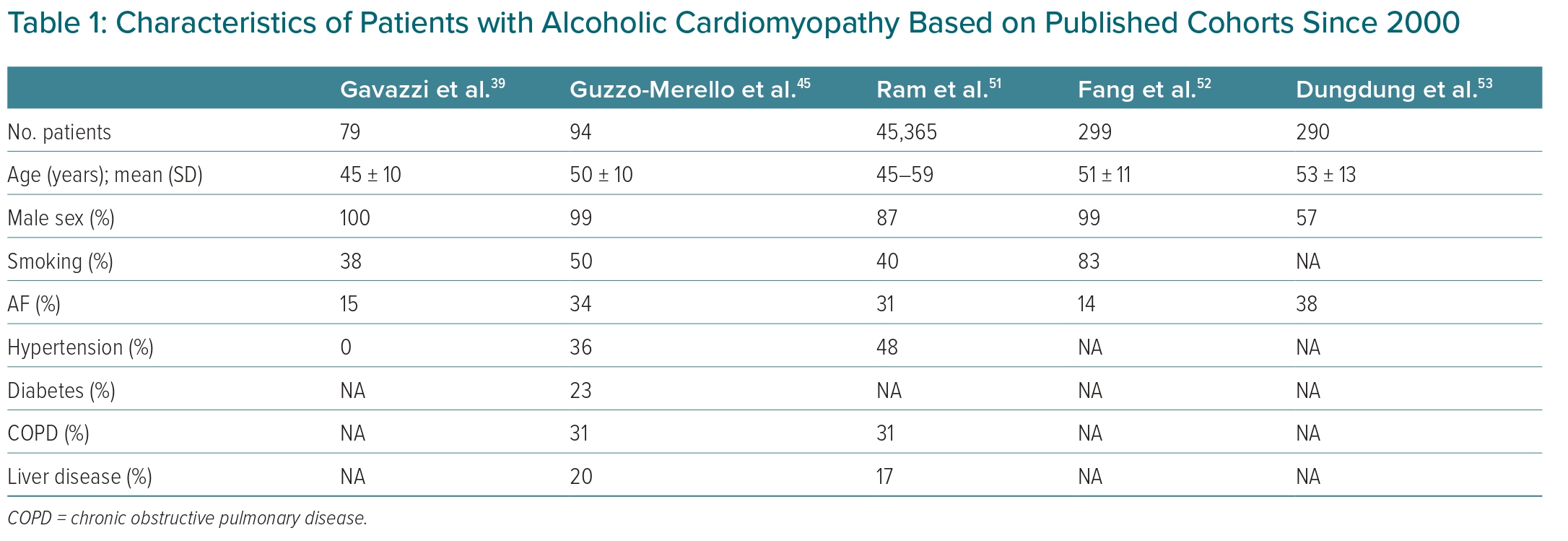
Concomitant factors, such as smoking, chronic obstructive pulmonary disease, hypertension and AF, in patients with alcoholic cardiomyopathy are commonly reported in the published literature (Table 1).39,45,51–53
Alcohol, AF and Arrhythmias
Cardiac arrhythmias are intrinsically linked with heart failure, whereby one condition contributes to the other. Alcohol consumption has long been associated with arrhythmogenesis, even in those with normal cardiac function, and among studies examining this, AF appears to be the most common alcohol-induced arrhythmia.20 Other types of arrhythmias commonly seen are atrial flutter, isolated ventricular premature beats, multiple supraventricular beats and paroxysmal atrial tachycardia.20
The arrhythmogenic effect of alcohol was demonstrated in a prospective study of a Swedish population, which concluded that alcohol consumption, even at a moderate, regular intake (>1 drink/week), increased the risk of developing AF.25 That study found that the relative risk of AF increases by 10% for each drink per day. Among moderate drinkers, binge drinkers were found to have a 29% increased risk of developing AF compared with non-binge drinkers.25 The Framingham Study sought to ascertain whether long-term alcohol consumption was associated with an increased incidence of AF among 10,333 participants.54 After adjusting for potential confounders, it found a 34% increased risk of AF among participants who consumed >36 g/day alcohol.54
Comparing those who drank >6 drinks/day with those consuming <1 drink/day, Cohen et al. demonstrated that the RR was at least doubled for each of AF, atrial flutter, supraventricular tachycardia and atrial premature beats.55 Given the paucity of evidence comparing the relationship between alcohol and ventricular arrhythmias, Tu et al. studied 408,712 middle-aged Britons over a median follow-up time of 11.5 years and concluded that there was no clear association between alcohol consumption and incident ventricular arrhythmias.56 However, the authors did note a statistically significant increased risk of ventricular arrhythmias in those consuming >14 drinks of spirits per week, but not with any other type of alcoholic beverage.
Correlation versus Causation
What makes correlation and causation between alcohol consumption and cardiovascular disease difficult is the association with a wide variety of cardiovascular conditions that are all different in disease characteristics. Conditions such as A-DCM, systemic hypertension, supraventricular tachycardias, AF, cerebrovascular accidents, coronary artery disease and heart failure are all inherently different disease processes, but are all intrinsically linked to each other in one form or another. Furthermore, because heart failure can occur in the later stages of the above cardiovascular conditions or due to general population longevity, the association between alcohol consumption and heart failure is confounded further. For example, although the aforementioned Mendelian randomisation study concluded that alcohol was not associated with increased risks of heart failure, it did find increased risks of stroke and AF.37 This makes examining the interrelationship between cerebrovascular accidents, alcohol consumption and AF difficult to examine and quantify at an epidemiological level.
Despite high alcohol use, not every individual develops A-DCM, indicating an underlying varying susceptibility by some people. This can be an environmental factor or based on an individual’s other lifestyle choices, such as diet, smoking and level of activity, but lends credence to a possible underlying genetic component. A recent study has found variants in well-characterised dilated cardiomyopathy (DCM)-causing genes were more prevalent in patients with A-DCM than control subjects.57 It also identified an interaction between a titin (TTN) genotype and excess alcohol consumption in a cohort of DCM patients not meeting A-DCM criteria. On multivariate analysis, DCM patients with the titin truncating variants (TTNtv) who consumed excess alcohol had an 8.7% absolute reduction in ejection fraction compared with those without TTNtv and excess alcohol consumption.
In addition, cardiovascular dysfunction has been described in non-alcoholic cirrhotic liver disease.58 Patients with non-alcoholic cirrhosis have been found to have increased plasma and total blood volumes, increased resting heart rate, enlarged left atrial and left ventricular volumes and normal to raised pulmonary artery pressures with increased pulmonary blood flow.59 Patchy fibrosis and myocardial oedema may affect the stiffness of the myocardial wall and result in impaired left ventricular filling and diastolic dysfunction.59 A reduction in cardiac function has also been shown in patients with jaundice, with or without cirrhosis, suggesting that circulating bile salts can inhibit cardiac contractility.60 Thus, evidence suggests that ‘cirrhotic cardiomyopathy’ differs from A-DCM and complicates the continuum further.
Conclusion
The association between alcohol consumption and cardiovascular disease is complex. Although heavy alcohol use has been shown to be intrinsically linked to A-DCM, less than heavy consumption is not as clearly incriminated in the literature. In most cohort studies, the consumption of small to moderate amounts of alcohol has not been linked to heart failure, suggesting a threshold effect of alcohol influenced by the background of the individual, possibly genetic predisposition rather than a continuous effect of exposure. It remains unclear whether alcohol intake can affect non-alcohol-related heart failure. The conventional belief is that A-DCM is the most common cause of DCM, but this evidence is based on small clinical samples (n<400) of patients with DCM with higher alcohol congestion in one-quarter of patients. There are no case-control series or community-based studies to support this and, when combining this lack of data with the absence of a specific clinical diagnostic parameter to differentiate between DCM and A-DCM, it casts further doubt on the association.
Furthermore, studies have suggested that A-DCM can be reversed with abstinence, but this is from smaller cohort studies assessing LVEF in isolation. In contrast, studies have shown irreversible histological damage and fibrosis in A-DCM, and we know that patients with idiopathic DCM can improve their LVEF with conventional medical therapy. Thus, it is plausible that A-DCM forms a continuum were mild–moderate cases with myocardial inflammation without fibrosis are the cases that can be reversed with conventional therapy and abstinence, whereas cases with irreversible histological damage and fibrosis may require advanced heart failure management in the form of device therapy, LVAD or heart transplant (if no contraindications).
In contrast, certain cardiovascular risk factors have a clear association with alcohol consumption. As described, alcohol consumption increases the risk of systemic hypertension and there is an association, in particular with binge drinking, with atrial arrhythmias and AF.
From a global health perspective, the topic of alcohol consumption garners great interest due to longstanding use of alcoholic beverages in our societies despite the obvious risk of medical and social harm from overindulgence. According to the WHO, because ‘any alcohol use is associated with some short-term and long-term health risks, it is difficult to define universally applicable population-based thresholds for low-risk drinking’.61 Based on current literature and evidence, one can only deduce and prescribe broad-statement advice in relation to alcohol consumption. Furthermore, here we have only explored the potential cardiovascular risks of alcohol consumption, but it would be remiss not to consider the impact of alcohol on other organ systems, mental health and wellbeing when assessing the true risks of alcohol consumption.
Overall, based on the breadth of the evidence on population and societal levels, we can conclude that the deleterious effects of alcohol consumption outweigh any potential beneficial effects. Individual patient advice should be limited to avoiding alcohol overuse and treating alcohol misuse and addiction aggressively; aiming to reduce alcohol to no more than nationally agreed upper limits of consumption; and, if a patient is a moderate user of alcohol, reviewing their case on a patient-level basis, as well as all contributing factors to their cardiovascular disease including diet, weight, smoking and social circumstances, and optimising clinical risk factors, such as hypertension.