Dyslipidaemia plays a major role in the pathogenesis of atherosclerosis and has become a permanently evolving area of clinical interest. Scientific societies periodically publish international guidelines for use as recommendations for daily practice in different regions of the world.1
Dyslipidaemia is a constantly changing field as a consequence of advances in understanding of the pathophysiological mechanisms of the relationship between lipid metabolism and atherogenesis, along with the development of new, potent, lipid-lowering therapies.2,3 Thus, concepts such as atherogenic dyslipidaemia or residual risk have become common subjects of analysis in the recent medical literature.4 Beyond LDL cholesterol, suboptimal levels of other atherogenic lipids and lipoproteins – including triglycerides, HDL cholesterol, non-HDL cholesterol (total cholesterol minus HDL cholesterol) and apolipoprotein B – also play a role.5
Statin Therapy: The Gap Between Guidelines and Real-world Clinical Practice
Statins, ezetimibe, the birth of proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors and the rebirth of fibrates and omega 3 fatty acid therapies, have contributed to debate about the gap between theoretical guidelines and clinical practice in the real world. The recently published EUROASPIRE V survey showed that a large majority of patients in primary care at high cardiovascular risk failed to achieve the lifestyle, blood pressure, lipid and glycaemic targets defined in the 2016 joint European societies’ guidelines, illustrating the wide gap that still exists.6 Despite the powerful concept of high cardiovascular risk in terms of mortality and events and the importance of achieving lipid goals, gaps in dyslipidaemia care have been reported among patients with established cardiovascular disease (CVD).7,8
Okerson et al. conducted a retrospective cohort study in 90,287 patients in the US with a diagnosis of clinical atherosclerotic CVD (ASCVD).9 The aim of the study was to evaluate the impact on clinical practice of the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines.9 Their main finding was that statin use remained the same before and after the publication of the guidelines. There were no changes in mean LDL cholesterol levels. In patients who had received high-intensity statins, statin use increased by 4% 1 year after the guidelines (p<0.001). In addition to these poor preliminary data, there was also criticism towards the guidelines as they changed the main concept: LDL targeting to treatment based on the level of risk, and of the fact that the score proposed by the AHA/ACC overestimated the risk in regions outside the US.10 However, many years later, we have recognized the main contribution of guidelines.
Statins are recommended by the UK’s National Institute for Health and Care Excellence (NICE) as first-line lipid-modifying therapy for the reduction of cardiovascular event risk in patients with ASCVD, as well as diabetes, familial hypercholesterolaemia, chronic kidney disease and other high-risk primary-prevention populations.11 Taking into consideration the availability of generic atorvastatin, the NICE guidelines recommended atorvastatin 80 mg for patients with ASCVD and atorvastatin ≥20 mg for those with most other high-risk conditions. However, in a cohort study that included 91,479 patients with ASCVD, 21% did not receive any statin and only 31% received a high-intensity statin.12 Up to 94% of patients with ASCVD and 85% of high-risk non-ASCVD individuals – representing approximately 3 million individuals in each group in the UK – would require statin up-titration or initiation to achieve full concordance with updated guidelines.
The REPAR study was a multicentre, prospective observational study in Spain including 1,103 patients with stable coronary heart disease.13 Only 26% of patients had LDL cholesterol <1.8 mmol/l, while 55% received low- or moderate-intensity statin therapy. When patients had LDL cholesterol values >1.8 mmol/l the attitude of physicians was passive. Over 70% made no changes, 26% increased treatment and 3% decreased it. The authors identified differences according to age of physicians – with a more proactive attitude in older doctors – and by region, unrelated to patient profile.
Problems in achieving lipid goals and applying guideline recommendations are not restricted to European and North American countries. The PURE study reported a low proportion of patients with coronary artery disease or antecedent of stroke treated with statins in South America (18% and 9.8%, respectively) and in South Asia (4.8% and 0.6%, respectively).14,15
The cross-sectional observational ICLPS was conducted in 452 centres in 18 countries in Eastern Europe, Asia, Africa, the Middle East and Latin America, recruiting more than 9,000 patients.16 Patients who had been receiving a stable dose and type of lipid-lowering therapy for ≥3 months before enrolment and had their LDL cholesterol value measured while receiving stable lipid-lowering therapy in the previous 12 months were eligible. The percentage of patients who achieved the relevant target goals was 51.4% when estimated by physicians versus 39.9% when based on European Society of Cardiology (ESC)/European Atherosclerosis Society recommendations (p<0.001), demonstrating an important gap between guidelines and clinical practice. Overall findings in patients receiving stable lipid-lowering therapy from countries outside western Europe suggest that approximately one-third of very-high-risk patients and half of high-risk patients achieve their risk-based target goals, whereas over half to two-thirds of moderate-risk patients achieve their goal.
Evidence supports the importance of the use of ezetimibe added to statin therapy to achieve goals and reduce events and cardiovascular risk. The results of the landmark IMPROVE-IT indicated that after acute coronary syndrome, ezetimibe 10 mg/simvastatin 40 mg was superior to simvastatin 40 mg alone in reducing cardiovascular events in high-risk patients.17 A reduction of recurrent events was observed. Patients with diabetes, prior stroke and prior coronary artery bypass graft appeared to have a greater treatment effect from ezetimibe than patients without diabetes. However, ezetimibe prescription is still lower than expected.
In the FOURIER study population, 27,564 patients with established CVD and at least one major risk factor (diabetes, current smoking, age ≥65 years, MI or non-haemorrhagic stroke, or symptomatic peripheral artery disease) were treated with lipid-lowering therapy.18 At baseline, only 1,440 (5.3%) were receiving ezetimibe.
More recently, the REDUCE-IT trial randomised 8,179 statin-treated patients with elevated triglycerides (≥3.5 mmol/l and <13 mmol/l), LDL cholesterol (>1.0 mmol/l and ≤2.6 mmol/l) and a history of atherosclerosis (71% of patients) or diabetes (29% patientsof ) to icosapent ethyl 4 g/day or placebo.19 Only 6.4% of patients were given ezetimibe.
The VIPFARMA ISCP Project
Apart from statin intensity and LDL cholesterol goals, there are some aspects of atherogenic dyslipidaemia that are often neglected.20 It is well known that atherogenic dyslipidaemia is associated with poor cardiovascular outcomes, but markers of this condition, such as triglycerides, are often ignored in clinical practice.21
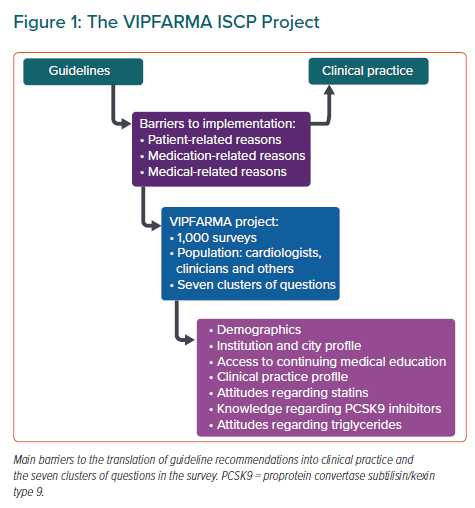
Some aspects explain the barriers to implementing recommendations from guidelines into clinical practice worldwide. A decade ago, Erhardt et al. grouped the components of non-adherence into patient, physician and medication-related reasons.22 In order to improve continuing medical education programmes, it is essential to understand causes that relate to clinician attitudes. This underpins the rationale for the International Society of Cardiovascular Pharmacotherapy (ISCP) Surveillance of Prescription Drugs in the Real World Project (VIPFARMA ISCP; Figure 1).
Aim
The aim of the VIPFARMA ISCP survey is to obtain relevant and representative data on a specific population regarding prescriptions or adherence to pharmacological therapeutic protocols. In the first stage, the ISCP will focus on the pharmacological management of lipid disorders.
The pilot research will be conducted by the Argentinean chapter of the ISCP. Because updated Argentinean guidelines are yet to be published, the ESC 2019 recommendations will be used as a reference.23 While lifestyle habits regarding dyslipidaemia are recognised as crucially important, this study will focus on medical attitudes towards lipid-lowering drug therapies.
Methods
Study Design
A cross-sectional online survey will be submitted to doctors in different specialties (internal medicine, cardiology, endocrinology, general medicine or other) who usually treat patients with dyslipidaemia in the range of 1–10 patients per week. Participants specify their sub-specialty when responding (preventive medicine, preventive cardiology, diabetes, arterial hypertension or other). Our research team will send personal invitations to peers and will post open invitations on social media. The pilot study aims to reach 1,000 returned surveys in Argentina. Reminders will also be sent.
The questionnaire will include 30 questions with dichotomous, Likert-scale, rank-order, and open-ended response choices (Supplementary Material Appendix 1). Questions will not be compulsory and respondents will be permitted to select multiple response choices depending on the question content.
Statistical Analysis
Data will be collected via Google Forms and exported to SPSS (version 24.0; IBM) for statistical analysis. Means and SD will be used for continuous variables and frequencies and percentages for categorical variables. Independent sample t-tests will be used to compare the normally distributed continuous variables, the Mann–Whitney U test will be used for non-normally distributed continuous variables, and the Pearson χ-squared test (or the Fisher’s Exact test, as appropriate) for categorical variables. A p value <0.05 will be considered statistically significant.
Survey Content and Rationale
Demographics
This cluster of questions focuses on age, sex, number of years of practice, specialty and subspecialty. The PERCRO-DOC survey, conducted among 1,382 randomly selected physicians (general practitioners/family medicine specialists, internists and cardiologists) from different regions of Croatia, showed that primary care physicians generally use their own personal experience in prevention, while internists and cardiologists are more likely to use guidelines.24
Another aspect we will ask about is the possible influence of pharmaceutical marketing on the dissemination of guideline content and about the use of new drugs.25 In 2019, the ESC board published a position statement that highlighted the changes resulting from its new Codes of Practice for the Pharmaceutical and Medical Device Industry.26 Consequently, access to scientific updates could probably be facilitated in specific subgroups.
Institution and City Profile
The PURE study demonstrated clear differences between urban and rural populations regarding cardiovascular prevention treatments.27 Therefore, it is relevant to analyse the differences in attitude and knowledge of doctors according to institution characteristics, the size of their cities where they work and the geographical location. Disparities in access to training and education of healthcare professionals, in conjunction with societal factors, may contribute to significant differences in morbidity and mortality from CVD in cities and provinces of the same country.28
Access to Continuing Medical Education
Clinicians in today’s healthcare environment face an overwhelming volume of information, which requires continued education and lifelong learning. In order to determine access to continuing medical education, questions focus on academy activities, subscription to medical journals and recent reading of scientific articles. A Cochrane review of educational meetings examined 81 randomised controlled trials and concluded that there are differences in the improvement of professional practice and the health outcomes of patients according to the type of educational activity to which healthcare professionals have access.29 Nissen et al. demanded changes in the continuing medical education system due to the accelerating rate of change in medical knowledge, which represents an enormous challenge to physicians’ ability to offer patients high-quality care.30,31 Barriers to access these new educational platforms can determine different degrees of knowledge and application of the guidelines in clinical practice.
Clinical Practice Profile
These questions aim to determine the experience in the management of patients with two types of lipid disorders, both of which involve a high cardiovascular risk condition: familial hypercholesterolemia and atherogenic dyslipidaemia in secondary prevention patients. The first is usually under diagnosed and the second is associated with inadequate treatment.32,33 In particular, early identification of familial hypercholesterolaemia is important for the prevention of coronary artery disease.34 Frequency of care in this group of patients could determine professional behaviour in terms of the goal level to be proposed and the intensity of the treatments they will be comfortable to indicate.35 The experience of the physician may possibly be reflected in the type of decisions that they take in specific patients, such as those with familial dyslipidaemia.36
Attitudes Regarding Statins
Despite the large and consistent body of evidence on the benefits of statins in primary and secondary prevention, their proper use continues to be a huge challenge for public health.37,38 Misconceptions lead to medical decisions with undesirable consequences, such as non-adherence to treatment, insufficient doses or failure to reach goals. For this reason, these questions will ask about the clinicians’ experience of adverse effects and the combination of statins with other drugs, such as ezetimibe.17
Knowledge Regarding PCSK9 Inhibitors
Understanding of PCSK9 has revolutionised the management of dyslipidaemia and has prompted research into monoclonal antibodies that inhibit it, such as alirocumab and evolocumab.39,40 While these drugs are included in the new guidelines, the opinion of physicians on these high-cost biological drugs is unknown, particularly regarding the very low LDL cholesterol fraction that can be achieved. In the FOURIER trial, 48-week outcomes showed that LDL cholesterol level in the evolocumab group was reduced to ≤1.8 mmol/l in 87% of patients, to ≤1.0 mmol/l in 67% of patients and to ≤0.65 mmol/l in 42% of patients. This compared with 18%, 0.5%, and <0.1%, respectively, in patients in the placebo group (p<0.001 for all comparisons, evolocumab versus placebo). The questions in this cluster are designed to establish the level of confidence and any concerns that physicians have regarding the use of these drugs.41
Attitudes Regarding Triglycerides
The final cluster of questions will address the attitude of physicians towards the interpretation and management of elevated triglycerides. It is now established that omega-3 and omega-6 fatty acids play important roles in human health and disease. Recent results from REDUCE-IT have impacted medical opinion because it addressed residual risk, finding a significant 25% relative risk reduction in first ischaemic events using icosapent ethyl 4 g daily versus placebo in statin-treated patients with triglycerides ≥135 mg/dl.42 Finally, we will ask about cut-off values to treat hypertriglyceridaemia and prescribing of fibrates or omega 3 fatty acids.
Conclusion
Dyslipidaemia plays a critical role in the pathogenesis of atherosclerosis. Proper pharmacological management of lipid disorders, especially familial and atherogenic dyslipidaemia, constitutes one of the greatest challenges in cardiovascular prevention in high-risk patients. However, some medical barriers prevent patients from achieving goals, contributing to the perceived gap between guidelines and daily clinical practice. It is therefore relevant to determine the attitudes of physicians regarding lipid management. The results of the VIPFARMA ISCP project will allow the identification of obstacles that exist in the medical community and the setting of an agenda to improve continuing medical education programmes.
Click here to view Supplementary Material.