Athletes may occasionally succumb to sudden cardiac arrest because of a quiescent cardiac abnormality. These catastrophes are rare, affecting between 1 in 17,000 to 1 in 50,000 athletes, depending on the sporting discipline.1,2 Most deaths affect male athletes participating in explosive sports of a start–stop nature, such as basketball and soccer, and occur during or immediately after exercise.1 The visibility afforded by such deaths generates considerable concern in the lay public, because young athletes are considered to represent the healthiest segment of society. Furthermore, there are several acceptable interventions to modify the natural history of these diseases and minimise the risk of sudden cardiac death.2,3
Over the past two decades there has been a growing momentum to provide cardiac evaluations in young athletes competing in the highest echelons of sport.3–6 Concurrently there has been an explosive increase in ethnic diversity in sport. Athletes from around the world now perform at the highest level in a multitude of sports. Therefore, the ethnic component of cardiovascular adaptation to exercise has become increasingly relevant, particularly in pre-participation screening. A thorough knowledge of these differences is highly pertinent for the practicing cardiologist because some athletes, especially black men, reveal electrical repolarisation changes and/or echogenic features, as part of a normal ethnic variant that overlaps with cardiac disease.7,8
This short review will examine ethnic differences in cardiac adaptation to sport. Most data are available in white athletes. There is also a wealth of data in athletes of African or Afro-Caribbean origin. However, smaller studies in athletes from other ethnicities are also included for comparison.
Cardiac Adaptation in White Athletes
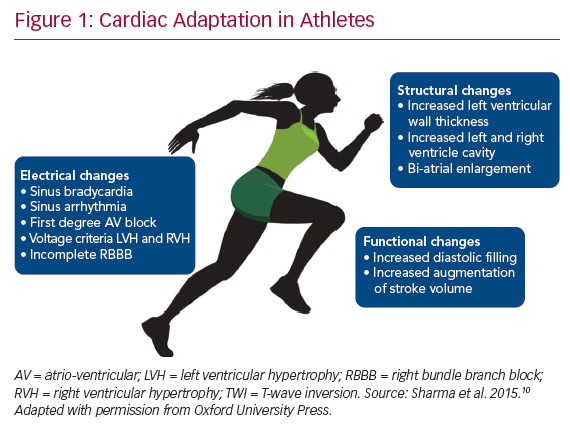
Participation in regular systematic intensive physical training is accompanied by an alteration in autonomic tone and increase in cardiac size, both of which have an impact on electrocardiographic and cardiac imaging studies in athletes (Figure 1).7,9 The magnitude of these adaptations, described as the ‘athlete heart’, are governed by several factors including age, sex, ethnicity, type and intensity of sport, and – notably – ethnicity.10
Electrical Adaptation
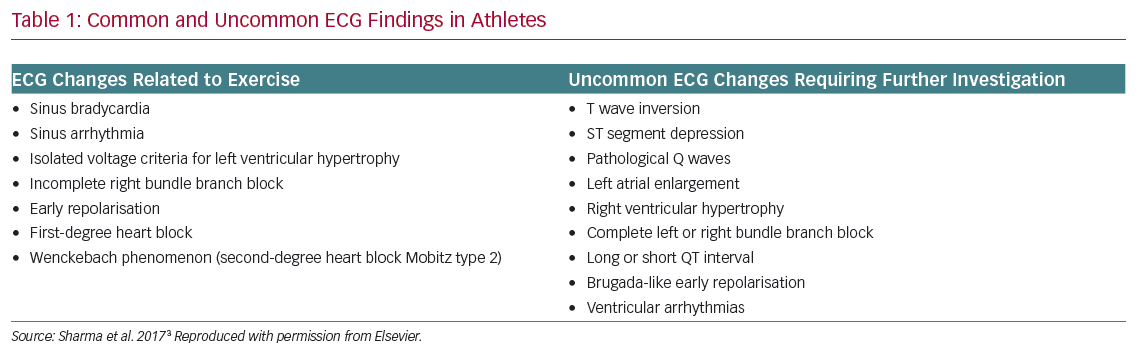
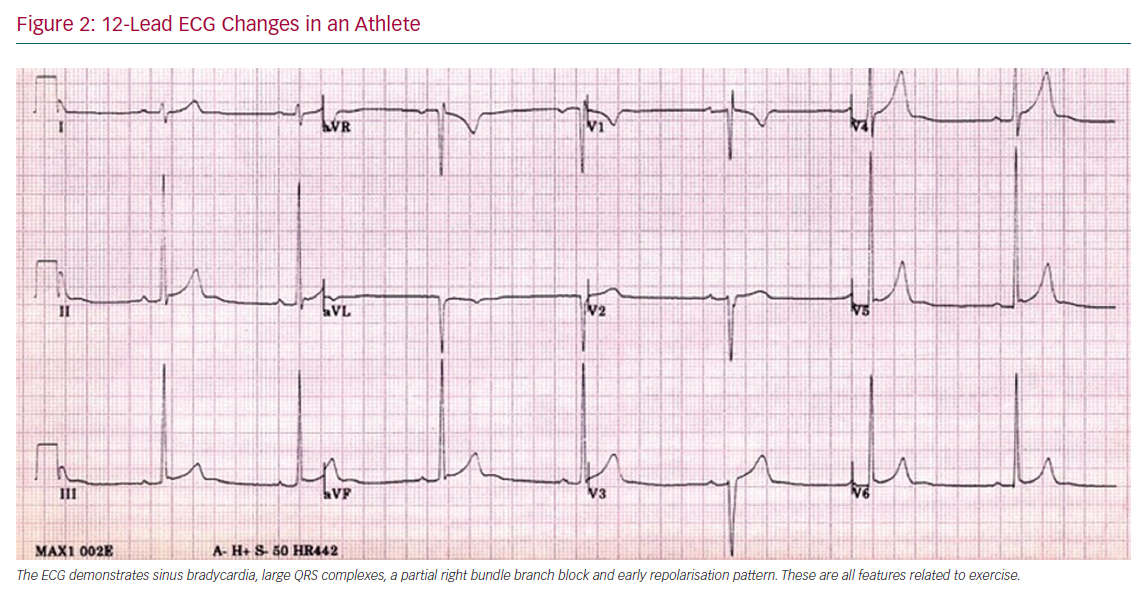
The electrical manifestations of the athlete heart broadly reflect increased vagal tone and a relative increase in cardiac dimensions.7,10,11 Sinus bradycardia, sinus arrhythmia, first degree atrio-ventricular block, large QRS voltages, incomplete right bundle branch block and early repolarisation are common in athletes of all ethnicities (Figure 2).10 In 2010, the European Society of Cardiology (ESC) provided recommendations for investigating athletes following a 12-lead ECG, whereby normal changes were classified as group one and abnormal changes were classified as group two (Table 1).12 These classifications were derived from a white population of >30,000 Italian amateur athletes, with some entering sports competition for the first time. Hence, these recommendations are appropriate for the white population, but did not account for ethnic variations.12
Structural Adaptations
Structural data derived from large cohorts of white athletes have shown that athletes reveal a 10–20% increase in left ventricular wall thickness (LVWT) measurements and a 10–15% increase in ventricular cavity size compared with sedentary counterparts.13,14 Female athletes have smaller dimensions compared with male athletes in all ethnicities, but show the same qualitative changes as male athletes when they are compared with relatively sedentary female controls.15–17 LVWT >12 mm is rare in white athletes, although a significant proportion (14%) reveal a LV diameter of >60 mm.14 These features are generally confined to large men competing in endurance sports.14,18 Similar to adult white athletes, male adolescent athletes show a greater LVWT compared to female athletes of similar age. However, the degree of LV cavity increase in adolescent athletes is smaller compared to adult athletes.19 Changes in LV volume are mirrored in the right ventricle.20 A very small proportion of athletes show an aortic root diameter >40 mm.21
Black Athletes
Electrical Adaptation
Athletes of African and Afro-Caribbean (black) origin have a higher prevalence of voltage criteria for left ventricular hypertrophy (LVH), right ventricular hypertrophy (RVH) and atrial enlargement compared to white athletes. Black athletes also reveal a higher prevalence of repolarisation anomalies affecting the J point, ST segments and T waves.22,23 According to the 2010 ESC recommendations, black athletes are 2.5 times more likely to exhibit an abnormal ECG suggestive of pathology than white athletes (40.4% and 16.2%, respectively).24 These data prompted researchers to refine ECG criteria for ECG interpretation in athletes.25,26
Early Repolarisation Pattern and ST-segment Morphology
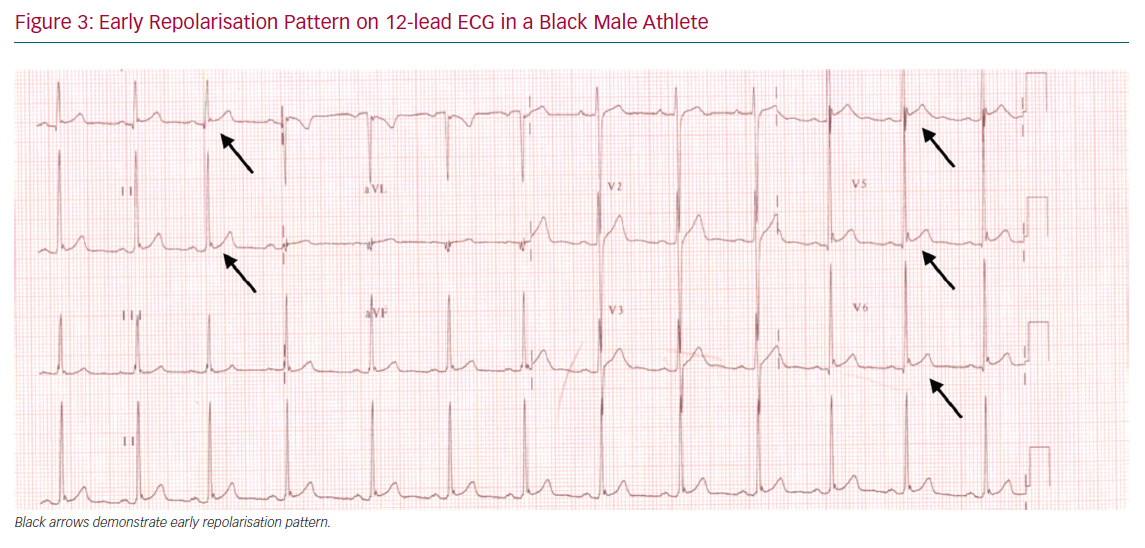
Early repolarisation (ER), defined as J point elevation ≥0.1 mV in the inferior and/or lateral leads, is more prevalent in black athletes compared to non-black athletes (34% versus 28%, respectively).27 Most black athletes reveal the ER in the lateral lead where the accompanying ascending concave ST-segments (Figure 3). The J point elevation may be >0.2 mV. Among athletes the ER pattern is frequently associated with increased voltage criterion for LVH, LV mass and relative wall thickness (RWT).28
In 2008, Haïssaguerre et al. reported that ER in the inferolateral leads was associated with idiopathic VF. However, few participants were athletes or black.29 Noseworthy et al. investigated 879 college athletes and showed that among athletes of all ethnicities, the ER pattern was more prevalent in male black athletes and – in multivariate analysis – was also associated with increased QRS voltage and slower heart rate, both markers of intensive physical training.30 Athletes frequently demonstrate an upsloping or ascending ST-segment type that is benign.31,32 One hypothesis proposes that parasympathetic modulation increases regional electrophysiological differences and repolarisation dispersion leading to ST-elevation.33 However, the ER pattern in the inferior, associated with higher J wave amplitudes (≥0.2 mV) and demonstrating horizontal or down sloping ST-segment after the J wave are associated with an increased risk of arrhythmic death in athletes and the general public.29,30,34
ST elevation is more common in black athletes than white athletes.22 Over 60% of black athletes reveal ST-segment elevation compared with 25% of white athletes. The ST-segments show a convex pattern in the anterior leads and a concave pattern in the inferior and lateral leads. Indeed, 40% of black athletes demonstrate convex anterior ST elevation in leads V1–V4.22,35 This pattern can be differentiated from the type 1 Brugada ECG pattern by measuring the amplitude at the J point (STJ) and 80 ms after (ST80). Athletes have ST-segment elevation after the J point whereas the ST-segment comes down after the J point in Brugada syndrome, therefore a STJ/ST80 ratio <1 suggests early repolarisation whereas a ratio >1 characterises a type one Brugada pattern. ST-segment depression is exceedingly rare in athletes irrespective of ethnicity and warrants further investigation to exclude structural cardiac disease.22
Anterior T Wave Inversion
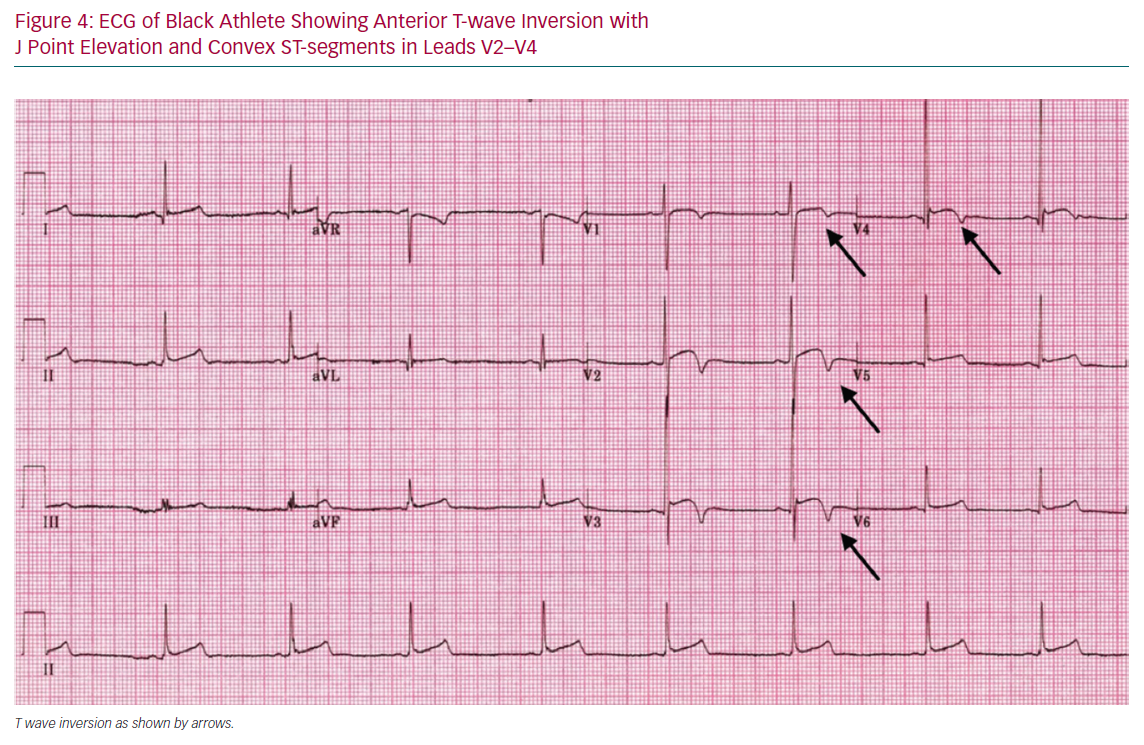
Anterior T wave inversion in leads V1–V4 on 12-lead ECG is common in the black population, with a prevalence of 12.7% of athletes and 4.2% in black controls compared with 1.9% in white athletes.22 Moreover, black male endurance athletes have an even higher prevalence of anterior T wave inversion – affecting one in five athletes – and is predicted by maximum LVWT.22
Anterior T wave inversion in black athletes is classically associated with J point elevation and convex ST elevation. T wave inversion is usually asymmetric with a steep downward slope, as illustrated in Figure 4. Detailed investigation of black athletes with anterior T wave inversion preceded by J point and convex ST segment elevation, including imaging studies, exercise stress test and prolonged ECG monitoring, have failed to identify an underlying abnormality.22,36,37 In our experience, anterior T wave inversion resolves within 6 weeks of detraining. Genetic studies using large gene panels to identify pathogenic variants causing cardiomyopathy and ion channel diseases have failed to identify any pathological abnormalities in black athletes with this repolarisation abnormality.38 Based on these observations, anterior T wave inversion preceded by J point and ST-segment elevation is considered a normal ethnic variant.3,22,35
Anterior T wave inversion is also recognised in arrhythmogenic right ventricular cardiomyopathy (ARVC). However, a study involving 80 healthy athletes with T wave inversion and patients with hypertrophic cardiomyopathy (HCM) and ARVC indicated that in contrast with healthy athletes, black individuals, including athletes with ARVC, show J point elevation <0.1 mV and isoelectric or depressed ST-segments preceding the T wave inversion in the anterior leads.39
Inferior T Wave Inversion
A study involving over 900 black athletes and 1,819 white athletes indicates that the prevalence of inferior T wave inversion (leads II, and aVF on 12-lead ECG) in black athletes is four times that of white athletes (6% versus 1.5%).22,40 Although current recommendations support further investigation of athletes with inferior T wave inversion, the precise significance of this repolarisation anomaly in black athletes is uncertain. Our own experience suggests that inferior T wave inversion is also more common in adolescent black athletes and we have yet to detect cardiac pathology in a black athlete with T wave inversion confined solely to the inferior leads.35,41 It is possible that this anomaly may be an ethnic variant but further large-scale studies are warranted.35
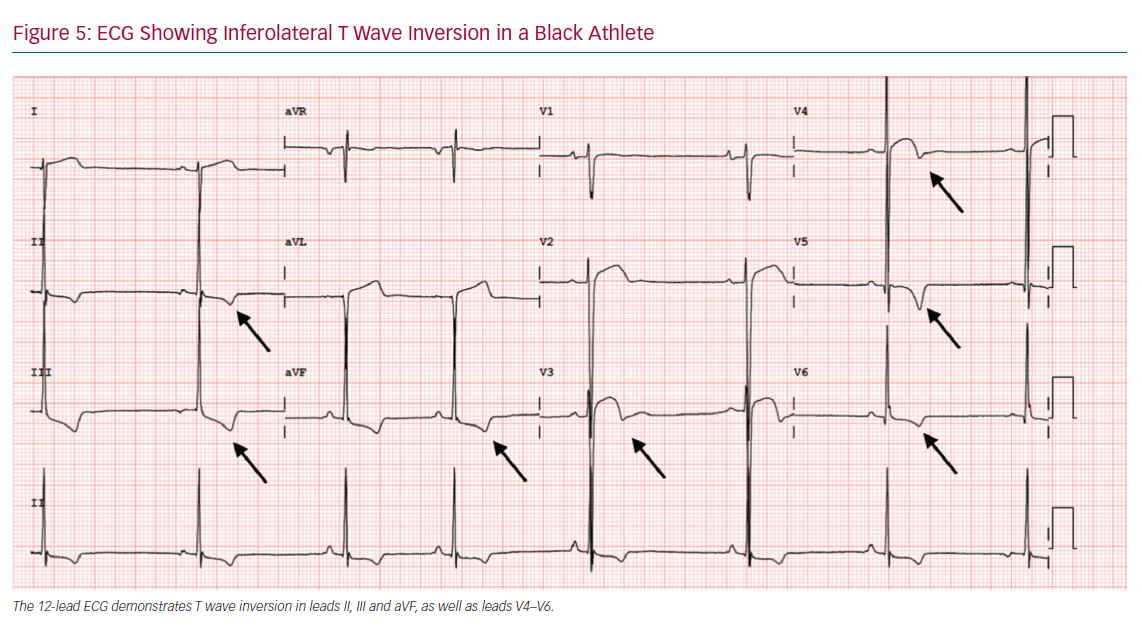
Lateral T Wave Inversion
Lateral T wave inversion (lead I and aVL, V5 and V6) occurs with a similar prevalence in sedentary and athletic black individuals (3–4%) and is 10 times more common than in white athletes.22 One study also showed that the prevalence of lateral T wave inversion in adolescent black athletes was also considerably higher than in white counterparts (2.4% versus 0.3%) (Figure 5).35 It is unlikely that all black athletes with lateral T wave inversion are destined to develop a cardiomyopathy. However, it is important to note that lateral T wave inversion is also a very common feature in black individuals with HCM (76.9%).22 Although the diagnostic yield of cardiomyopathy in black athletes with lateral T wave inversion is considerably less than in white athletes, one study showed that up to 18% of black athletes with lateral T wave inversion have an underlying cardiomyopathy.42 Therefore, all black athletes with lateral T wave inversion should be investigated as comprehensively as white athletes.42
Structural Changes
In general, black athletes undergo a similar process of exercise-related structural cardiac adaptation as white athletes.8 The effect of ethnicity on left or right ventricular cavity size between black and white athletes is minimal, with black athletes demonstrating marginally smaller proximal right ventricular outflow tract and longitudinal dimensions.8,43 Some studies have reported slightly larger left atrium and aortic dimensions compared to white athletes. However, there are a few notable structural differences.8,22
Black athletes generally exhibit a larger body surface area (BSA) and systolic blood pressure (SBP) than white athletes.22 Black male athletes demonstrate an increased LVWT ≥12 mm compared to white male athletes (12.4% versus 1.6%, respectively).22 Maximal LVWT >16 mm is rare in all athletes. One study showed that female black athletes also reveal an increased LVWT compared with white athletes. In this study investigating 240 nationally ranked black female athletes and 200 white female athletes, 3% of black athletes had a LVWT >11 mm compared to none of female athletes. None of the women revealed a LVWT >13 mm.36
Adolescent black athletes demonstrate a 5% increase in mean LVWT compared to white Italian athletes of a similar age (9.7 mm versus 9.2 mm, respectively).37
Concentric LV remodelling or hypertrophy is more prevalent in black male, female and adolescent athletes than their white counterparts.44–46 Haemodynamic responses to exercise have been proposed as a possible mechanism. One study showed that black adolescent athletes exhibit a higher SBP on exercise compared to white athletes.46 Furthermore SBP at peak exercise is a predictor of LV mass. However, ultimately ethnicity was the main determinant of RWT with a significant increases in LV wall thickness and mass suggestive of concentric remodelling.46 Delineating between physiological LVH and pathology is integral as American autopsy data suggest that HCM may go unrecognised in black athletes as the number dying suddenly from HCM is significantly greater than African-Americans diagnosed with HCM in hospital settings.47
LV hypertrabeculation is more prevalent in black than white athletes (28.8% versus 16.3%; p=0.002), specifically in athletes who participate in dynamic sports. Hypertrabeculation combined with T wave inversion may be suggestive of LV non-compaction. The use of cardiac MRI, exercise stress testing and prolonged ECG monitoring along with clinical assessment after a period of detraining can provide valuable information in differentiating pathology from physiological adaptation.48
Impact of Geographical Origins
The term ‘black athletes’ used throughout the literature encompasses a vastly diverse group of individuals spanning American football players, Brazilian soccer players and Kenyan long-distance runners. Riding et al. attempted to evaluate the role of geographical origin on electrical and structural adaptations in black athletes. In this novel study, they subdivided 1,698 male athletes into north, east, middle and west African, African-American/Caribbean, South American and west Asian groups.44
The large diversity in geographical origin directly affected the pattern of cardiac adaptation, with west and middle Africans having significantly more abnormal ECG findings as per the 2017 international recommendations (9.2% and 11.9%, respectively).44 Specifically, middle and west Africans demonstrated more T wave inversion compared to other black athletes (8.5% and 6.4%, respectively). Absolute wall thickness ≥12 mm was more common among African-American/Caribbean (9.5%), middle African (5.5%) and west African (4.9%) groups. However, when indexed to body size, LVWT was only significant in the middle and west African groups.44
It is not unexpected that athletes from the west and central Africa have similar patterns of cardiac adaptation. The Bantu expansion of people from west to central Africa explains the cultural and language similarities between these people and presumably their shared ethnicity and genetics.49 A criticism of the study is the lack of genetic testing to determine true genealogy and the effect of mixed heritage. Furthermore, there was no female participation in the trial.50
Studies in Athletes of Other Ethnicities
There are a limited number of studies examining cardiovascular adaptation in other ethnicities and almost all have focused on male athletes.
West Asians
Electrical Changes
Few studies have examined cardiac adaptation to exercise in athletes of west Asia. Wilson et al. assessed 800 male west Asian athletes with 135 controls, 300 black and 120 white athletes against the 2010 ESC recommendations.51 The authors did not find any significant differences in the incidence of abnormal ECGs between west Asian athletes and white athletes (1.6% and 0%, respectively).51 A recent study showed that, as with white athletes, west Asian adolescent athletes 11–18 years old demonstrate a lower prevalence of anterior T wave inversion beyond lead V3 than black adolescent athletes (0.7% v 7.0%), respectively.52 Conversely, Riding et al. found increased abnormal T wave inversion in west Asians compared to white south Europeans in a much smaller sample size. However, this did not correspond with any structural differences on echocardiography.44
Structural Changes
Arab athletes demonstrate increased LV mass and wall thickness compared with sedentary controls. However, absolute cardiac structure parameters are significantly smaller than both white and black athletes.53 There is no significant difference between LVWT between Arab and white athletes with a similar percentage demonstrating LVH (0.5% and 0.6%, respectively).53 To our knowledge, there are no studies on west Asian female athletes, making this an area that requires further research.
South and Far East Asian Athletes
Studies on South Asian athletes are exceedingly rare. A study of more than 18,000 South East Asian multi-ethnic male conscripts undergoing preparticipation screening for the Singapore armed forces showed a higher prevalence of voltage criterion for LVH in Chinese participants.54 A study of 351 Chinese athletes from the Han population suggested that 4.5% demonstrate an abnormal ECG requiring further evaluation.55 Echocardiography seems to correlate well to previously reported echocardiographic findings in white athletes in both men and women. Only three male athletes (1.76%) revealed a LVWT >12 mm.55
Carre et al. described a study of Japanese professional footballers that showed no difference between ECG abnormalities in Japanese athletes and white athletes. Eccentric LV remodelling was more common in Japanese athletes with an enlarged LV cavity when corrected for BSA compared to black and white athletes.56 A study of Japanese ultra-marathon runners also suggested that Japanese ethnicity is associated with larger LV end diastolic dimensions however this showed a significant correlation with age and years of exercise in a cohort of athletes with a much higher age range than previous mentioned studies.57,58
More research is required in the Far East Asian populations, particularly for female and adolescent athletes. However, existing evidence suggests that male Far East Asian athletes undergo a similar process of cardiac adaptation to white athletes with similar ECG interpretation.
Pacific Islanders
Pacific Islanders are indigenous people from Polynesia, Micronesia and Melanesia. A pilot study suggested that Pacific Islander rugby league players had increased LV mass and RWT when compared to white players as a result of cardiac adaptation.59 A larger study of 2,281 Pacific Islanders that included 716 women (mean age 19.4 ± 6.5) evaluated the differences between Melanesian, Polynesian, white and Métis athletes.60
Melanesians demonstrated significantly more T wave inversion compared to white men (2.6% versus 1.5%). The authors suggest that Melanesians have ECG patterns similar to black athletes. Unfortunately, not all participants with abnormal ECGs could have echocardiography or MRI scans, which may have increased the detection of cardiomyopathies. However, an increased prevalence of rheumatic valve disease (1.5%) was noted to be 3.9-fold higher than that reported in western and Middle East countries.60,61
Pre-participation Screening
The previous (2010) ESC recommendations for ECG interpretation in athletes were associated with a high false-positive rate in black athletes, with two in five requiring further investigation.24 The Seattle and refined 12-lead-ECG criteria maintained the same sensitivity of the ESC recommendations while improving the specificity for black athletes to 18.4% and 11.5% respectively.24 When compared to the Seattle criteria, the 2017 international ECG recommendations further reduced the number of ‘abnormal’ 12-lead ECGs from 3% to 1.6%, false positives and maintained sensitivity when reviewed by a sports cardiology expert.62 In adolescent black athletes, the international recommendations outperform the ESC recommendations.63
Both the Seattle criteria and the latest international recommendations account for some repolarisation anomalies and normal ethnic variants in black athletes. However the abnormal ECG rate remains considerably higher than in white athletes.64 In contrast, limited data from other ethnicities suggest that athletes of Asian origin reveal similar ECG patterns to white athletes.54,55 Screening with the international guidelines significantly reduces false positive rates for pathology in white athletes and, therefore, probably in Asian athlete cohorts. Nevertheless the false-positive rate in black athletes remains relatively high, despite the increased specificity (97%) compared to the ESC and Seattle criteria.64,65
Mixed Ethnicity
Our experiences and preliminary data on adolescent ‘mixed’ ethnicity footballers, specifically white and African descent, suggest phenotypical similarities with black athletes. Mixed athletes demonstrated significant increases in LVWT and prevalence of T wave inversion compared to white athletes but to a lesser extent than in black athletes.66
Conclusion
Ethnicity is an important determinant of cardiac adaptation to exercise and should be considered during cardiac evaluation of an athlete. Black athletes from middle and west Africa and the Caribbean appear to develop the most profound electrical and structural changes. An awareness of these ethnic variants will prevent over investigation of healthy athletes and potentially unwarranted exclusion from competitive sports.
Widespread pre-participation screening practice is fertile ground for research in ethnicity-specific cardiovascular adaptation to intensive exercise and has the potential to fill the gaps in our current body of knowledge. This information combined with long term surveillance of asymptomatic athletes with currently perceived ‘abnormal’ ECG findings will influence future recommendations on screening and expand our understanding of cardiac adaptation.