The current coronavirus disease 2019 (COVID-19) outbreak is more than a health crisis, and its impact on the management of other diseases of various specialties is one of the greatest challenges facing healthcare professionals. Health associations worldwide are now recommending dealing with emergencies only, utilising telemedicine and providing ambulatory facilities, where available, for non-emergency conditions to control the pandemic.
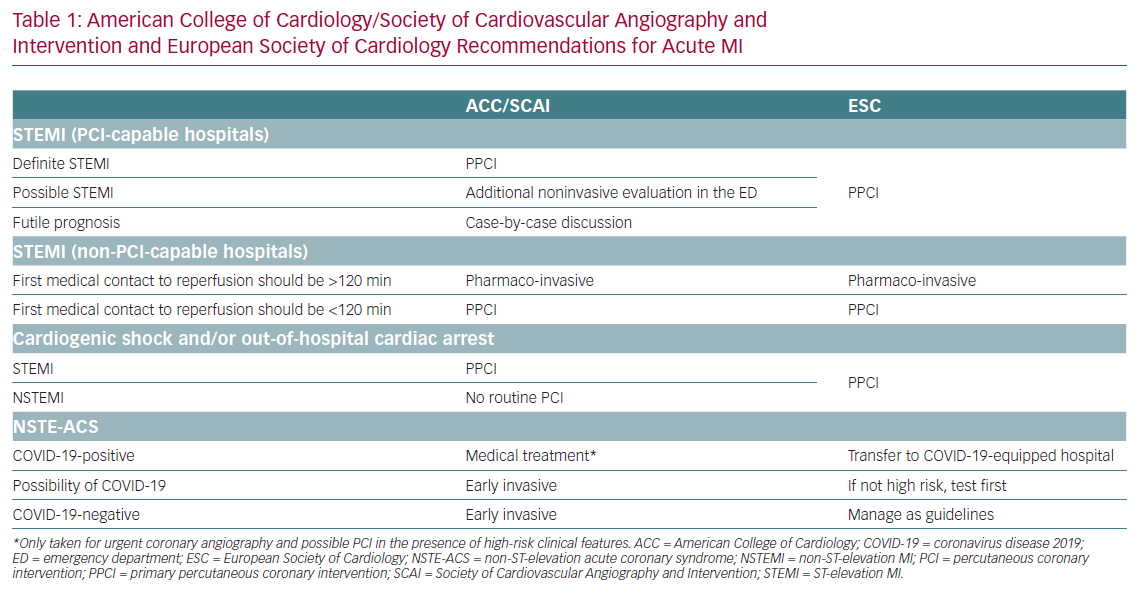
Interventional cardiologists are frontline workers who deal with many cardiovascular emergencies among suspected or confirmed COVID-19 patients. They are not only responsible for ensuring adequate protection against the infection, but also for the efficient utilisation of resources when considering non-emergency procedures. Many recognised international heart associations, including the American Heart Association and European Society of Cardiology (ESC), are currently setting appropriate recommendations for the management of emergency cardiac interventions (Table 1).1–3
Elective cases can be easily postponed to later dates after weighing risks versus benefits to avoid the exposure of patients to the hospital environment, where COVID-19 may be more prevalent, and to minimise exposure to healthcare workers and to preserve hospital bed capacity and other resources. Examples include percutaneous intervention for stable ischaemic heart disease, peripheral arterial disease procedures, atrial septal defect closure or left atrial appendage closure.1,4
During the COVID-19 pandemic, primary percutaneous coronary intervention (PCI) remains the standard of care for ST-segment elevation MI (STEMI) patients at PCI-capable hospitals when it can be provided in a timely fashion, with an expert team outfitted with personal protective equipment (PPE) in a dedicated catheterisation laboratory (cath lab). A fibrinolysis-based strategy may be used at non-PCI-capable referral hospitals or in certain situations where primary PCI cannot be executed or is not deemed to be the best option.2
In certain circumstances, a more detailed and confirmatory evaluation in the emergency department (ED) might be required prior to transfer to the cath lab. Thus, during the COVID-19 pandemic, there may be longer door-to-balloon (D2B) times. D2B times should still be tracked; however, patient and/or system-related delays are considered appropriate reasons for delay.2
Every patient who needs cardiac catheterisation must be screened at presentation.5 The WHO provides guidance for the risk stratification of patients at low to high risk of infection of COVID-19.6 Together with relevant history and examination, this can aid in taking appropriate protective measures when dealing with patients with, or at risk of COVID-19. Healthcare professionals must be provided with personal PPE, including respirators, a fluid-impermeable gown, head cover, gloves, splash goggles and shoe covers, whereas patients should wear a surgical mask from ED until intervention completion, or even until the discharge.7
Confirmed or suspected COVID-19 patients requiring intubation should be intubated prior to arrival at the cath lab, and the threshold for intubation may need to be lowered to avoid emergency intubation in the cath lab leading to aerosolisation of respiratory secretions.1
Radial access is the preferred approach over femoral access, because it keeps the primary operator at a greater distance from the patient’s face, reducing the possibility of aerosol transmission, and takes less time.8
For non-ST segment elevation acute coronary syndrome (NSTE-ACS), the treatment strategy must be tailored according to Global Registry of Acute Coronary Events (GRACE) scoring, as well as to the risk of being infected with COVID-19. Chest CT and swab tests should be immediately performed for suspected cases, and if necessary, coronary CT angiography (CCTA) done at the same time. Strict isolation should be started immediately for all ACS patients. If results are negative for COVID-19, then the patient can be transferred to the coronary care unit.9
According to the ESC guidelines for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, the management and treatment pathways for NSTE-ACS are categorised according to the risks to every patient.3
Patients with troponin elevation and no acute clinical signs of instability (i.e. ECG changes or recurrence of pain) could be managed with a primarily conservative approach. Non-invasive imaging using CCTA might speed-up risk stratification and avoid an invasive approach, allowing early discharge.10 For patients at high risk, the medical strategy is aimed at stabilisation and planning an early (<24 hours) invasive strategy. However, the time of the invasive strategy may be greater than 24 hours and depends on the timing of the test results. If feasible, a dedicated area to manage these patients while waiting for test results should be arranged in the ED. In the case of a positive COVID-19 test, patients should be transferred, for invasive management, to a hospital equipped to manage COVID-19-positive patients.3
It is best to dedicate one cath lab for COVID-19 patients.11 The cath lab must be fully equipped and the healthcare professionals should have proper PPE inside the lab, avoiding unnecessary entry and exit during the procedure.12
It is strongly recommended that procedures for donning and doffing of PPE are followed.7,12 It is important to minimise the number of in-lab healthcare professionals and to ensure that all doors are closed; for communication outside the lab, a microphone system should be used. Maintaining physical distance during the procedure as much as possible is also an important consideration.11 In cases where a patient requires resuscitation while in the cath lab, automatic chest compression devices are recommended.11 If unavailable, hands-only cardiopulmonary resuscitation (CPR) has been shown to be as effective as conventional CPR in many cases.13
For suspected or confirmed COVID-19 STEMI patients, there are two options: fibrinolytic therapy or primary angioplasty. Fibrinolysis is favored in China for their local conditions and because of the risk of staff contamination. In China, experts dealing with the COVID-19 pandemic recommend fibrinolytic therapy over PPCI for STEMI and especially for stable patients, as lytic therapy is less resource-intensive for the system overall.14,15 The same is not true in Europe, where the superiority of PPCI over thrombolysis is well-established and where efficient networks between the hub and spoke centers are active.16
As soon as the procedure is completed, the patient should be transferred to a dedicated isolation area. If no anteroom is available, the doffing of PPE must be done inside the lab, with the exception of the facial respirator, which should be removed outside of the lab. After waste disposal according to protocols, the lab should be closed for an hour before thorough cleaning to reduce the possibility of aerosol transmission. Cleaners must be fully equipped with PPE. All disposable material should be safely discarded. Surfaces can be disinfected by using sodium hypochlorite at a concentration of 1,000 parts per million, leaving it in contact with the surface for 5 minutes.7
It is preferable that medical staff, cardiology advance trainees and fellows, consultants, nursing staff, radiographers and cardiac technologists form teams that can work on a rotating basis in shifts, secluding ones from frontline care who are immunocompromised, have a chronic illness or are aged >65 years with comorbidities.11
Considering the care pathway for STEMI at referral hospitals (non-PCI centres), the decision to proceed with an initial fibrinolysis or a direct transfer to a PCI centre is multifactorial and will likely vary in different regions. The treatment decision also depends on whether the patient is COVID-19 positive or suspected of having COVD-19, and should be made between the referring hospital physician and PCI centre physician. Upon transfer of a patient with a STEMI from a referral hospital to a PCI centre, the patient should be re-evaluated for COVID-19 status and STEMI diagnosis. The patient can then be taken for primary PCI, pharmaco-invasive PCI or rescue PCI, as indicated.2
Once primary PCI is performed on the infarct related artery, if clinically safe and indicated, any high-grade disease in a non-infarct related artery should also be treated during the index procedure to minimise further exposure of the cath lab staff during a staged procedure. Primary PCI is superior for establishing normal thrombolysis in MI grade 3 coronary flow compared to an initial fibrinolysis strategy, and has a significantly lower risk of fatal and non-fatal bleeding complications.17 Furthermore, after a fibrinolysis-based strategy, just over 50% of patients are reperfused, resulting in a high proportion of patients requiring rescue PCI.17 This can result in prolonged intensive care unit (ICU) hospitalisation, with exposure to multiple healthcare providers, limiting access to ICU beds for COVID-19 patients. In addition, some of these patients may have a ‘STEMI mimicker’, such as focal myocarditis or stress cardiomyopathy known to be associated with COVID-19.18,19 Fibrinolysis of these patients would provide no benefit to the patient, but still incur bleeding risk and eventual invasive diagnostic catheterisation given that the ST-elevation is unlikely to resolve.
Ideally, a dedicated cath lab should be located in a COVID-19 area of the hospital, but this might not always be possible. In the latter case, a temporary COVID-19 lab and procedure with a protected team needs to be set up for each patient; this might require a longer time. If the cath lab is not ready, we suggest that patients wait in the ambulance, rather than in the pre-operating room.20
Finally, the safe reintroduction of cardiovascular interventional procedures during the COVID-19 pandemic can be achieved according to response level. Primary PCI should be introduced for most STEMI patients, and selective pharmaco-invasive therapy as per regional practice. If a patient has COVID-19 or there is a moderate-to-high probability of a patient being COVID-19 positive, consider alternative investigations (transthoracic echo and/or CCTA) prior to cath lab activation or pharmaco-invasive therapy. In high-risk ACS (non-STEMI/unstable angina), an invasive strategy is the treatment of choice, particularly when there are refractory symptoms, haemodynamic instability, significant left ventricular dysfunction, suspected left main or significant proximal epicardial disease and a GRACE risk score >140.21
The COVID-19 pandemic has had a global impact on the way in which healthcare systems operate. Frontline healthcare professionals put themselves at risk when treating patients. Excellent leadership, proper cath lab preparation, teamwork, mutual trust, regular updates, feedback and communication between multidisciplinary departments are essential during the pandemic.