Ischaemic heart disease (IHD) has been estimated to affect 126.5 million people globally.1 It is the global leading cause of premature disability and death.2,3 The classical cause of IHD is obstructive coronary artery disease (CAD) in the epicardial coronary arteries. However, other causes of IHD are at least equally important and increasingly recognised, including coronary vasomotor disorders.4–6 Approximately 70% of patients with angina and suspected myocardial ischaemia show no signs of obstructed coronary arteries after coronary angiography but still demonstrate ischaemia.7 Ischaemia with no obstructive coronary artery disease (INOCA) is increasingly acknowledged as a serious condition because of its association with poor quality of life and elevated risk for adverse cardiac events.8,9 There is only partial understanding of the pathophysiology of INOCA. In four in five INOCA patients, microvascular angina and/or vasospastic angina are observed, which are phenotypes of coronary vasomotor disorders.10–12 These can cause myocardial ischaemia by mismatching the supply and demand of myocardial blood flow and nutrients relative to the requirements of the heart.10,11 Coronary microvascular dysfunction (CMD) causes endothelial dysfunction and structural changes leading to a higher microvascular resistance in these smallest branches of the coronary arteries.9,13 Coronary artery spasm (CAS) is the sudden focal or diffuse narrowing of (epicardial) coronary arteries due to smooth muscle hyperactivity.14 CMD and/or CAS can ultimately result in myocardial ischaemia and acute coronary syndromes.
Risk Factors for Coronary Vasomotor Disorders
The risk factors for coronary vasomotor disorders remain partly unclear. Studies have shown an association between CMD and the traditional cardiovascular risk factors, such as smoking, age, diabetes, hypertension and dyslipidaemia.15,16 Sex differences are important in INOCA. Women are more likely than men to have INOCA with or without coronary vasomotor disorders when presenting with myocardial ischaemia symptoms.17–20 An important risk factor that has been receiving more attention over the past years is psychological stress. Research has demonstrated how psychological factors like chronic stress, anxiety, depression and social stressors can negatively affect cardiovascular health.21–26 Of note is that the association between psychological stress and IHD is bidirectional, as both cause and consequence.
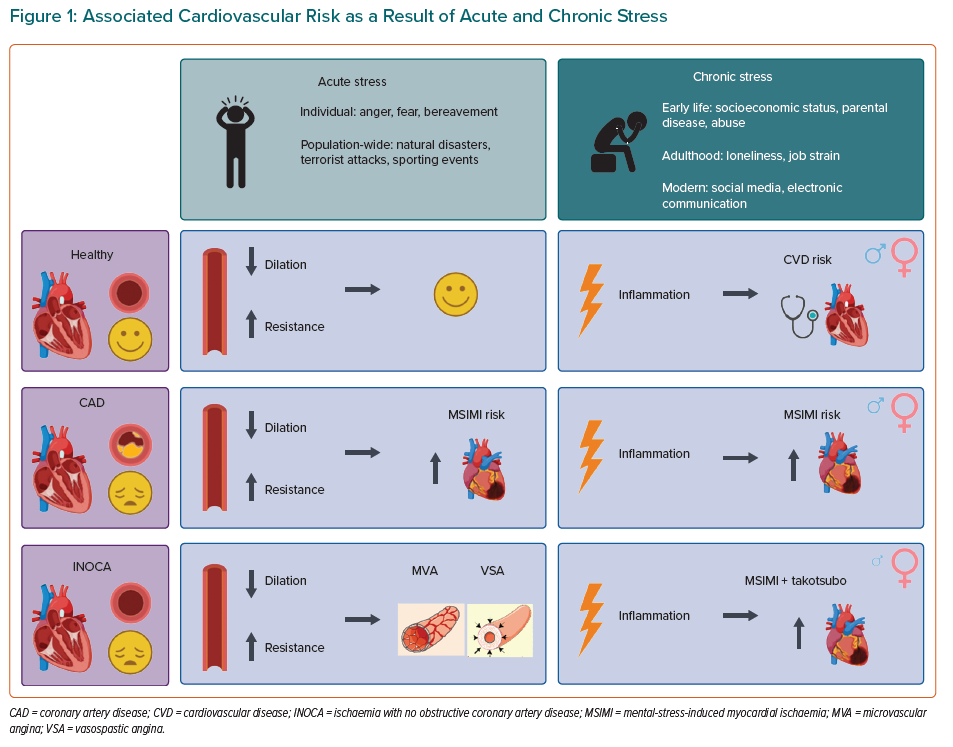
Acute mental stress causes an increase in heart rate, contractility and blood pressure. Normally, during mental stress the epicardial arteries and microvessels will dilate to increase coronary blood flow in order to match the increased demand of oxygen.27–29 In patients with obstructive CAD or INOCA, acute stress results in impaired dilation of the resistance vessels while the epicardial coronary arteries paradoxically constrict. Consequently, the demand cannot be met with increased coronary flow, which can ultimately lead to myocardial ischaemia.27–31
Many articles have been published regarding psychological stress and obstructive CAD, with varying results.29,32–37 However, only a few studies have looked specifically at INOCA patients.38–42 This review will provide an overview of the research on the effect of psychosocial stress in patients with INOCA and/or coronary vasomotor disorders. Furthermore, sex differences in pathophysiology will be described, as the impact of psychological stress is different between women and men.43
Definitions
Coronary Vasomotor Disorders
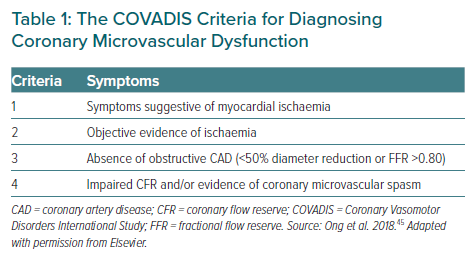
Microvascular angina can result from structural remodelling of the microvasculature and/or vasomotor disorders in the coronary arterioles. The definition and terminology of coronary vasomotor disorders and CMD has been clarified in recent years by the Coronary Vasomotor Disorders International Study group (COVADIS; Table 1).44,45
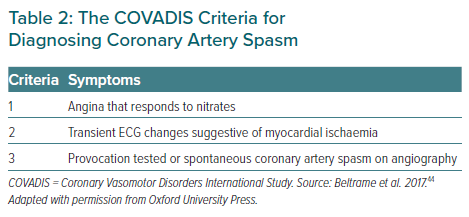
CAS leads to anginal chest pain – also named vasospastic angina – that cannot be distinguished from angina due to CMD.46 It is often underreported and underdiagnosed and can co-exist with (non-) obstructive CAD and/or CMD.14 Functional abnormalities of endothelial and vascular smooth muscle cells are a substrate of CAS.11 The COVADIS criteria for the clinical syndrome of CAS are presented in Table 2.44
INOCA Endotypes
INOCA is still underdiagnosed and undertreated. An important reason contributing to this is the lack of provocative spasm testing and measurement of microvascular resistance in clinical practice. Nevertheless, invasive testing is proven to be safe and should be used more widely to obtain an appropriate diagnosis for each individual patient.47–49 Invasive testing techniques include diagnostic guidewire and adenosine test and the acetylcholine test for vasoreactivity.50
The consensus document by Kunadian et al. describes five INOCA endotypes: microvascular angina; vasospastic angina, also named CAS; a combination of microvascular angina and vasospastic angina; non-cardiac chest pain; and non-flow-limiting CAD, which is described as diffuse atherosclerosis with <50% stenosis severity.50 Establishing the exact phenotype is important to be able to advise the most suitable medical treatment.
Types of Psychological Stress
Psychological distress – whether chronic or acute or both – has been linked to IHD risk.51,52 Chronic stress can originate both in early life, with causes that include poor socioeconomic status, parental illness and sexual abuse, but also in adulthood when loneliness and job-strain may play a role.53,54 Early-life traumas in particular seem to affect behavioural and lifestyle factors such as smoking and substance abuse and unhealthy eating habits. Other chronic psychological conditions include post-traumatic stress disorder, anxiety and depression.52 These severe chronic stress conditions impact neurobiological and cognitive functions, which negatively affect physical health. On the contrary, disorders caused by acute stress are mostly a result of a sudden spike of the major stress mediators in combination with a vulnerable background.54 Acute stress can be experienced on the individual level (e.g. anger, fear or bereavement) and/or population-wide level (e.g. natural disasters, terrorist attacks or sporting events).52,54
Studies have shown an increase in mental health issues in young adults over the past decade.55–57 In particular, the rate of anxiety, depression, suicidal ideation and self-injury in young adults is increasing. The emergence of digital media and electronic communication are thought to be contributors to this problem. Digital media seems to have the biggest impact on the younger generation by causing insecurities, anxiety and reductions in sleep duration.57
The Role of Psychological Stress in Patients with INOCA
In past decades, many studies have focused on the effect of types of psychological stress on IHD. Psychological stress can induce MI, as reported in the large INTERHEART study by Rosengren et al.33 In addition, having had a prior MI may also result in increased mental stress, so the association is therefore bidirectional. Acute stress seems to worsen endothelial function, increases arterial stiffness and induces microvascular constriction in patients with established CAD.37
Stress and the Coronary Microvasculature
The response of the coronary microvessels to mental stress is determined by endothelium-dependent coronary microvascular function. Furthermore, the response is reflected in the peripheral microvascular circulation.36 Endothelial dysfunction could be a mechanism for causing mental stress-induced myocardial ischaemia (MSIMI) in CAD patients.36 This arises at a lower workload compared to exercise-induced ischaemia and is associated with an increased risk of MI and cardiovascular death.34,58
Sex Differences
Young women with stable CAD have a higher chance of MSIMI than older women or age-matched men.58,59 Furthermore, young women with a previous MI have a twofold higher chance of developing MSIMI compared to men.60 Men and women appear to have different predictors for MSIMI. CAD severity and the rate-pressure product response to psychological stress are strong predictors for MSIMI in men, whereas among women peripheral vasoconstriction and CMD have been shown to be associated with MSIMI.60,61 Women were more likely to have a lower income, be ethnic minorities and have a history of sexual and emotional abuse.58,59 Psychological risk factors are considered a higher burden for women than men, especially in women with INOCA.39,58 Some studies suggest an association between a history of anxiety and INOCA, while others did not find a link between depression or general anxiety and INOCA. These associations remain to be further elucidated.39,62–64
CMD is often present in women with INOCA and endothelial dysfunction appears more frequently in young women as a response to psychological stress than in similar aged men.65–67 In the WISE (551 women) and the WISE-CVD (350 women) cohorts, the effects of home and work stress were investigated with additional measurement of financial stress in the second cohort. Both studies used comparable methods and showed significant associations between cardiac symptoms, CAD risk and psychological distress. One important difference between the cohorts was home/work stress being the stronger predictor for cardiovascular disease in WISE, and financial stress being the stronger predictor for cardiovascular disease in WISE-CVD.40 The WISE cohort also determined that CMD predicted MI, heart failure hospitalisation, stroke and death in these women.68 Moreover, patients with CMD had elevated mental stress-induced peripheral vasoreactivity.14
Stress and Microvascular Dysfunction in Takotsubo Syndrome
Women in particular are more vulnerable to MSIMI and a takotsubo syndrome when a significant physical or emotional stressor occurs.69,70 Multiple studies have shown the involvement of CMD in the pathogenesis of takotsubo syndrome.71–73 It is mostly observed in post-menopausal women without epicardial CAD.71 Women with a history of takotsubo syndrome show excessive vasoconstriction and impaired peripheral vasodilation after being exposed to acute mental stress.70,71 Studies suggest that an acute dysfunction of the coronary microvasculature might serve as a cause for takotsubo syndrome.70,71,73
Potential Effects of Stress in Coronary Artery Spasm
The exact role of psychological factors in CAS remains unclear, as there few studies in patients with only CAS. Psychosocial stress might play a role in inducing smooth muscle cells in the vasculature to become hyperactive as a result of autonomic nervous system dysfunction, which can lead to oxidative stress, inflammation and endothelial dysfunction.14 The neuroendocrine and autonomic nervous system appears to mediate these effects because certain brain areas contribute to autonomic outflow, emotional regulation and vascular reactivity.74 Imaging of the coronary arteries in patients with vasospastic angina showed a localised inflammation in the perivascular adipose tissue and coronary adventitia.75 Both epicardial coronary spasm and microvascular spasm seem to be mediated by rho-kinase.76 Potential triggers of these spasms include hyperventilation, autonomic imbalance and platelet activation.75
Because autonomic dysfunction and inflammation also play a role in the connection between psychological stress and IHD, it was hypothesised by Hung et al. that anxiety and depression may influence CAS.77 They studied the prevalence of history of anxiety and depression in 10,473 CAS patients, 10,473 CAD patients and 10,325 healthy individuals. They found a higher prevalence of anxiety and depression in patients with established CAS compared to patients with obstructed CAD (anxiety: OR 2.29; 95% CI [2.14–2.45], depression: OR 1.34; 95% CI [1.08–1.66]) and controls (anxiety: OR 5.20; 95% CI [4.72–5.74], depression: OR 1.98; 95% CI [1.50–2.62]). Most patients with CAS were younger women. However – even though this was a large study – no sex differences were found between the association of CAS with anxiety and depression.77 These observations show a possible involvement of CAS in the aetiology of INOCA through anxiety and depression.
Stress-reducing Therapies
Coronary endothelial dysfunction in patients with INOCA can serve as a therapeutic target for medical therapy (statins, angiotensin-converting enzyme inhibitors) and lifestyle interventions. Stress-reducing medication such as anti-depressants might reduce cardiac risk, but most studies to date have been underpowered to prove this.78 Stress-reducing therapies such as mindfulness-based interventions and meditation training might reduce types of psychological stress like anxiety while also decreasing blood pressure, non-fatal MI and cardiovascular mortality.78 Overall, stress reducing interventions seem to have a promising positive impact on psychological and cardiovascular health.
Stress and Inflammation in Women
An enhanced inflammatory state due to psychological distress increases inflammatory markers and subsequently the progression of CAD.79–84 The coronary microvascular response in INOCA patients seems to be modulated by the level of inflammation, even without the presence of conventional risk factors.85 Basal levels of interleukin (IL)-6 are higher in young women with CAD compared to age-matched men, and thus could have enhanced immune reactivity to stress.86 Levels of IL-6 increase in women with CAD after exposure to psychological stress. Furthermore, IL-6 levels are much higher in young women. Oestrogens and glucocorticoid sensitivity might play a role. Cytokine production may be enhanced by oestrogens, resulting in increased secretion of pro-inflammatory cytokines.87 This would also explain why IL-6 levels in post-menopausal women may be lower. However, the exact role of oestrogens in inflammation is still largely unknown. Rohleder et al. showed an increase in glucocorticoid sensitivity after 1 hour of mental stress testing in men but a decrease in sensitivity in women. Glucocorticoid sensitivity is important for inhibiting pro-inflammatory cytokine production. This means that in women, a decreased glucocorticoid sensitivity might enhance pro-inflammatory cytokine levels after acute psychological stress.88
Stress-related mental disorders like depression and post-traumatic stress disorder are more frequent in women than in men. The link between stress related disorders and IHD is closely related to behavioural and lifestyle factors such as smoking, substance abuse and poor diet. However, these do not entirely explain the connection between stress and IHD. Increased inflammation, hypercoagulability, endothelial dysfunction and genetic factors also play a role.89–91 For example, the association of depression and IHD is more often attributed to genetic factors in women than in men, where the heritability of depression is approximately 42% in women and 29% in men.92,93
Reproductive function might serve as another mechanism through which stress increases IHD risk in women. Stress is closely related to ovarian disruption, which is present in almost 20% of women during their reproductive years.94 Ovarian disruption increases the risk for IHD and thus women who are exposed to a lot of stress are thought to have increased IHD risk, in some ways, due to ovarian dysfunction.95 Because younger women are more susceptible to the adverse effects of psychosocial factors and MSIMI is more common in this group, the functional status of the ovaries might serve as a mechanism to the IHD risk in younger women.59
Conclusion
Acute and/or chronic psychological stress can lead to increased risk of cardiovascular diseases. CMD seems to be linked to psychological stress and depression, thereby increasing cardiovascular disease risk. CMD is prevalent in INOCA patients and might be considered as a contributing factor to mental-stress-associated adverse cardiovascular outcomes (Figure 1). It is important that future research regarding psychological stress and INOCA uses the consensus criteria of INOCA with standardised stress testing protocols and questionnaires. This offers the opportunity to compare studies, which could shed more light on this growing patient population.